Northland > Private Hospitals & Specialists >
Dr Mark Kennedy - Private Internal Medicine Specialist
Private Service, Internal Medicine, Cardiology, Respiratory, Gastroenterology, Hepatology
Today
8:00 AM to 4:30 PM.
Description
As a Specialist Physician, Dr Kennedy sees patients with a range of cardiology, respiratory/chest, upper GI (including non-viral liver), neurology, endocrinology, haematology, nephrology and rheumatology conditions. He has a broad range of interests including chest pain, ischaemic and valvular heart disease, cardiac rhythm disturbances, syncope, difficult hypertension, heart failure, cardiomyopathy, myocarditis, pericarditis, dyslipidaemia, gastro-oesophageal reflux, peptic ulcer, coeliac and liver disease. He is experienced in the management of chest diseases including asthma, cough, bronchitis, pneumonia, bronchiectasis, COPD, emphysema, respiratory failure, lung cancer, pleural disease, non-tuberculous mycobacterial disease, sarcoidosis, asbestos-related pleural disease, asbestosis, interstitial lung disease, Aspergillus lung disease, DVT, pulmonary embolism and disordered breathing/hyperventilation. He also cares for patients with cerebrovascular disease, headache, thyroid and non-viral liver disease (fatty liver, non-alcoholic steatohepatitis NASH, autoimmune hepatitis, primary biliary cholangitis etc), cirrhosis, haemochromatosis, polymyalgia rheumatica, giant cell arteritis, gout, inflammatory arthritis, fibromyalgia, haematological conditions, osteoporosis and fatigue.
Southern Cross Affiliated Provider for Cardiology
Southern Cross Affiliated Provider for Internal Medicine
Southern Cross Affiliated Provider for Gastroscopy
Southern Cross Affiliated Provider for Lung Function
Our team prides itself on a patient-focused, evidence-based approach to care.
We offer a broad range of procedures through the practice:
- ECG
- Exercise Tolerance Test (ETT) or Exercise Test/Exercise ECG
- Echocardiography (TTE or Echo), Bubble Study
- Exercise Stress Echocardiography (ESE)
- Coronary Artery Calcium Score
- Holter and Event Monitor
- 24-hr Ambulatory Blood Pressure Monitor (ABPM)
- Elective Synchronised Electrical Cardioversion
- Gastroscopy
- Liver Biopsy
- Spirometry including pre and post-bronchodilator
- Full Lung Function Testing, including Plethysmography, DLCO, Resting Minute Ventilation and FeNO
- Pleural Procedures
Dr Kennedy has been a Northland DHB Specialist General Physician since 1991, and has worked in private practice as a Specialist in Internal Medicine since 1996. He is New Zealand trained, and qualified as MBChB (Otago) in 1981, and attained the FRACP in 1987. He is affiliated with the Ascot Cardiology Group and is also a consultant in the General Medicine, Respiratory and Liver Services at Northland District Health Board. He has been involved in the care of patients in the Wards, Coronary Care and Intensive Care Units at Whangārei Hospital and at Northland's Private Kensington Hospital. He undertakes Public Hospital Clinics, seeing patients with General Medical, Respiratory, Cardiac, Hepatic and Upper Gastrointestinal disease.
Dr Kennedy offers the broadest range of investigative procedures of any of the Physicians in Northland.
Dr Kennedy works closely with a small, highly experienced team; Clinic Nurse Gemma at the Private Rooms, Nurses with Cardiology expertise with Exercise Testing, Michael an experienced Cardiac Sonographer and a Clinical Respiratory Physiologist.
What is a Specialist Physician or Internal Medicine Specialist?
A Consultant General Physician is a highly trained specialist who provides a range of non-surgical healthcare to adult patients. He cares for difficult, serious or unusual medical problems, when the diagnosis may be difficult. The General Physician's broad training provides expertise in the diagnosis and treatment of problems affecting different body systems, and in a variety of medical procedures essential for the diagnosis and management of severe and complex illness. Much of a General Physician’s work takes place with outpatients in clinics and with hospitalised patients, both private and public. A General Physician is frequently asked to review patients before surgery. He advises a Surgeon of a patient's risk status, and can recommend appropriate management to minimise the risk of any operation. The Physician can also assist with the management of on-going medical problems or complications following surgery. A General Physician sees patients who have been referred to him by other doctors, either the patient's General Practitioner or another Medical or Surgical Specialist.
Staff
1. Gemma - Clinic Nurse
2. Cathy- Practice Manager and Reception
3. Michael - Senior Cardiac Sonographer
4. Meika - Cardiac Nurse
5 Robin - Cardiac Nurse
6. Leisa - Cardiac Nurse
7. Scott - Respiratory/Sleep Physiologist
8. Elisa - Clinical Cardiac Physiologist
Consultants
-

Dr Mark Kennedy
Internal Medicine Specialist
How do I access this service?
Referral
A referral is required from your GP or Specialist for a consultation.
Referral Expectations
Your GP will refer you to Dr Kennedy if they feel you would benefit from a Specialist Physician's advice regarding your medical condition. You can also request a second opinion from your General Practitioner. A history of your symptoms, past medical and family history will be taken, and your medications will be checked. Any available old notes will be reviewed, you will be examined and your investigation results will be perused with you. Recommendations regarding your diagnosis and options for investigation and treatment will be discussed. A letter will be sent to your GP, with a copy to you. If you have any important change in your condition before you come to your appointment, please see your GP immediately.
What you need to bring to your appointment:
- Any relevant letters or reports from your Doctor, Hospital or other Specialist.
- All medicines you are currently taking, including herbal, natural, complementary preparations. Please bring the medications, including any inhalers.
- Local radiology is accessible on-line. Please bring x-ray, CT (Computed Tomography) or MRI (Magnetic Resonance Imaging) reports or images that may have been taken outside of Northland.
- A support person can be helpful.
What to bring to an Immigration Medical appointment:
- Immigration e-referral requesting that you are to see a Specialist (straightforward Immigration Medicals are undertaken by a Panel Physician, a GP nominated by NZ Immigration).
- All relevant current and previous x-ray, CT and MRI images and reports (if Immigration is still holding your overseas x-rays, please obtain the x-rays from them). Local radiology is accessible on-line.
- If English is not your first language, please bring someone who can interpret and speak on your behalf. A support person can be helpful, even if you speak fluent English.
- Your passport.
Fees and Charges Description
You can be advised of the costs of standard consultation and follow-up at the time of making your appointment. Additional charges for other procedures are also available on enquiry (ECG, Spirometry, Echocardiogram etc).
Dr Kennedy is a Southern Cross Affiliated Provider for Cardiology, Internal Medicine, Gastroscopy and Lung Function. This means that if you have medical insurance cover with Southern Cross, the claim will be submitted directly to Southern Cross for you and you will be informed whether there is a shortfall payment depending on your policy. Payment of any shortfall is expected on the day.
We see other insured and self-funded patients.
Payment is required at the time of appointments (whether or not you have insurance cover), unless by prior arrangement.
Payment accepted: Cash, EFTPOS, Credit Card (Visa, Mastercard) and Direct Credit/Internet Banking. We do not accept cheques.
Hours
8:00 AM to 4:30 PM.
| Tue – Fri | 8:00 AM – 4:30 PM |
|---|
Monday to Friday: 8 am - 4.30 pm for Reception. Nurse available: Monday 9 am - midday, Tuesday and Thursday 8 am - 5 pm. Closed weekends and public holidays.
Public Holidays: Closed Good Friday (18 Apr), Easter Sunday (20 Apr), Easter Monday (21 Apr), ANZAC Day (25 Apr), King's Birthday (2 Jun), Matariki (20 Jun), Labour Day (27 Oct), Northland Anniversary (26 Jan), Waitangi Day (6 Feb).
Common Conditions / Procedures / Treatments
Patient information: An ECG (Electrocardiogram) tracing is a recording of your heart's electrical activity that can be read by your doctor. It is a quick, easy, painless test that records the electrical signals generated by the heart with each heart beat. Electrode patches are attached to your skin over your chest and limbs to measure the electrical impulses given off by your heart. An ECG may be performed as a routine screening test (e.g. before surgery) or in people complaining of problems such as chest pain, palpitations, high blood pressure, or shortness of breath. It can provide important information about the heart rhythm, a previous heart attack, thickness of the heart muscle, heart chamber enlargement or strain, inadequate oxygen delivery to the heart, or problems with the conduction of electrical signals through the heart. The ECG procedure: Cardiac signals are detected by multiple electrodes (sticky pads), placed on the chest and limbs, and transcribed onto paper by the ECG machine. The procedure takes approximately 5 - 10 minutes. After the test: Dr Kennedy will interpret the ECG. It is important to note that a normal ECG does not exclude heart disease, and further testing may be necessary. Depending on your history, examination and ECG findings, you may go on to have other investigations such as echocardiography or some form of cardiac exercise testing.
Patient information: An ECG (Electrocardiogram) tracing is a recording of your heart's electrical activity that can be read by your doctor. It is a quick, easy, painless test that records the electrical signals generated by the heart with each heart beat. Electrode patches are attached to your skin over your chest and limbs to measure the electrical impulses given off by your heart. An ECG may be performed as a routine screening test (e.g. before surgery) or in people complaining of problems such as chest pain, palpitations, high blood pressure, or shortness of breath. It can provide important information about the heart rhythm, a previous heart attack, thickness of the heart muscle, heart chamber enlargement or strain, inadequate oxygen delivery to the heart, or problems with the conduction of electrical signals through the heart. The ECG procedure: Cardiac signals are detected by multiple electrodes (sticky pads), placed on the chest and limbs, and transcribed onto paper by the ECG machine. The procedure takes approximately 5 - 10 minutes. After the test: Dr Kennedy will interpret the ECG. It is important to note that a normal ECG does not exclude heart disease, and further testing may be necessary. Depending on your history, examination and ECG findings, you may go on to have other investigations such as echocardiography or some form of cardiac exercise testing.
Patient information:
An ECG (Electrocardiogram) tracing is a recording of your heart's electrical activity that can be read by your doctor. It is a quick, easy, painless test that records the electrical signals generated by the heart with each heart beat. Electrode patches are attached to your skin over your chest and limbs to measure the electrical impulses given off by your heart. An ECG may be performed as a routine screening test (e.g. before surgery) or in people complaining of problems such as chest pain, palpitations, high blood pressure, or shortness of breath. It can provide important information about the heart rhythm, a previous heart attack, thickness of the heart muscle, heart chamber enlargement or strain, inadequate oxygen delivery to the heart, or problems with the conduction of electrical signals through the heart.
The ECG procedure:
Cardiac signals are detected by multiple electrodes (sticky pads), placed on the chest and limbs, and transcribed onto paper by the ECG machine. The procedure takes approximately 5 - 10 minutes.
After the test:
Dr Kennedy will interpret the ECG. It is important to note that a normal ECG does not exclude heart disease, and further testing may be necessary. Depending on your history, examination and ECG findings, you may go on to have other investigations such as echocardiography or some form of cardiac exercise testing.
Patient information: An ECG undertaken when you are resting may be normal, even when you have coronary artery disease. An Exercise ECG is the most widely used screening test for cardiac disease and is an important and accurate way of assessing how the heart works when placed under a 'load'. Abnormalities of the heart are frequently recognised in this way. Most new patients, and many patients undergoing a 'follow-up' visit, will undertake an exercise test. The Exercise ECG is most commonly used to see if you have any evidence of coronary artery disease and can give your doctor some idea as to how severe your coronary artery disease might be. The Exercise test: Ten electrodes ('sticky pads') are applied to the chest, and a blood pressure monitor is placed on the arm. For this test you have to walk on a treadmill while your heart is monitored. The test starts at quite a slow pace, comfortable for the specific patient, though the treadmill gets slightly faster and steeper every 3 minutes. You can stop at any time, although the test is usually stopped if anginal pain occurs, any significant ECG changes occur or when an adequate exercise level and heart rate have been reached. This test is supervised by Dr Kennedy and his Cardiac Nurse and is interpreted both during and following the procedure. The ECG and blood pressure are used to monitor the patient during and after the test. The nurse and/or doctor assess the patient and the ECG for evidence of heart problems. During an exercise ECG the heart is made to work harder so that if there is any narrowing of the coronary arteries resulting in a poor blood supply and oxygen delivery to a region of heart muscle. It is more likely to be picked up on the tracing, as your heart beats more quickly and contracts more vigorously. The test is sometimes used to assess your exercise tolerance and your heart rate response to exercise. After the test: An exercise test that is clearly negative after a significant level of exercise is reassuring and indicates good cardiac function. The exercise test results can be used to direct further investigations and possible treatment.
Patient information: An ECG undertaken when you are resting may be normal, even when you have coronary artery disease. An Exercise ECG is the most widely used screening test for cardiac disease and is an important and accurate way of assessing how the heart works when placed under a 'load'. Abnormalities of the heart are frequently recognised in this way. Most new patients, and many patients undergoing a 'follow-up' visit, will undertake an exercise test. The Exercise ECG is most commonly used to see if you have any evidence of coronary artery disease and can give your doctor some idea as to how severe your coronary artery disease might be. The Exercise test: Ten electrodes ('sticky pads') are applied to the chest, and a blood pressure monitor is placed on the arm. For this test you have to walk on a treadmill while your heart is monitored. The test starts at quite a slow pace, comfortable for the specific patient, though the treadmill gets slightly faster and steeper every 3 minutes. You can stop at any time, although the test is usually stopped if anginal pain occurs, any significant ECG changes occur or when an adequate exercise level and heart rate have been reached. This test is supervised by Dr Kennedy and his Cardiac Nurse and is interpreted both during and following the procedure. The ECG and blood pressure are used to monitor the patient during and after the test. The nurse and/or doctor assess the patient and the ECG for evidence of heart problems. During an exercise ECG the heart is made to work harder so that if there is any narrowing of the coronary arteries resulting in a poor blood supply and oxygen delivery to a region of heart muscle. It is more likely to be picked up on the tracing, as your heart beats more quickly and contracts more vigorously. The test is sometimes used to assess your exercise tolerance and your heart rate response to exercise. After the test: An exercise test that is clearly negative after a significant level of exercise is reassuring and indicates good cardiac function. The exercise test results can be used to direct further investigations and possible treatment.
Patient information:
An ECG undertaken when you are resting may be normal, even when you have coronary artery disease.
An Exercise ECG is the most widely used screening test for cardiac disease and is an important and accurate way of assessing how the heart works when placed under a 'load'. Abnormalities of the heart are frequently recognised in this way. Most new patients, and many patients undergoing a 'follow-up' visit, will undertake an exercise test.
The Exercise ECG is most commonly used to see if you have any evidence of coronary artery disease and can give your doctor some idea as to how severe your coronary artery disease might be.
The Exercise test:
Ten electrodes ('sticky pads') are applied to the chest, and a blood pressure monitor is placed on the arm. For this test you have to walk on a treadmill while your heart is monitored. The test starts at quite a slow pace, comfortable for the specific patient, though the treadmill gets slightly faster and steeper every 3 minutes. You can stop at any time, although the test is usually stopped if anginal pain occurs, any significant ECG changes occur or when an adequate exercise level and heart rate have been reached. This test is supervised by Dr Kennedy and his Cardiac Nurse and is interpreted both during and following the procedure. The ECG and blood pressure are used to monitor the patient during and after the test. The nurse and/or doctor assess the patient and the ECG for evidence of heart problems.
During an exercise ECG the heart is made to work harder so that if there is any narrowing of the coronary arteries resulting in a poor blood supply and oxygen delivery to a region of heart muscle. It is more likely to be picked up on the tracing, as your heart beats more quickly and contracts more vigorously. The test is sometimes used to assess your exercise tolerance and your heart rate response to exercise.
After the test:
An exercise test that is clearly negative after a significant level of exercise is reassuring and indicates good cardiac function.
The exercise test results can be used to direct further investigations and possible treatment.
Patient information: Echocardiography is also known as cardiac ultrasound or echo. This test is performed by a highly experienced, fully qualified and dedicated Cardiac Sonographer, Michael Mooten. Echocardiography is a test that uses high frequency sound waves to generate pictures of your heart. During the test, you generally lie on your back and left side; gel is applied to your skin to increase the conductivity of the ultrasound waves. The cardiac sonographer then moves the small, plastic transducer over your chest. The test is relatively painless and can take from 10 minutes to half an hour. The machine analyses the information and develops images of your heart and these images are seen on a monitor. This is referred to as an echocardiogram. Echocardiography can help in the diagnosis of many heart problems including coronary artery disease, previous heart attacks, valve disorders, weakened heart muscle, holes between heart chambers and fluid around the heart (pericardial effusion). A bubble echocardiogram study can be undertaken to diagnose or exclude a hole in the heart. If your doctor is looking for evidence of coronary artery disease he may perform a variation of this test: Exercise echocardiography - a technique used to view how your heart works under stress. It compares how your heart works when stressed by exercise compared with when it is at rest. The ultrasound is undertaken before exercise and immediately after you stop exercising. A standard treadmill is used (see Exercise ECG above). After the test: An Exercise Stress Echo that is clearly negative is reassuring and indicates good cardiac function. The Exercise Test results can be used to direct further investigations and possible treatment.
Patient information: Echocardiography is also known as cardiac ultrasound or echo. This test is performed by a highly experienced, fully qualified and dedicated Cardiac Sonographer, Michael Mooten. Echocardiography is a test that uses high frequency sound waves to generate pictures of your heart. During the test, you generally lie on your back and left side; gel is applied to your skin to increase the conductivity of the ultrasound waves. The cardiac sonographer then moves the small, plastic transducer over your chest. The test is relatively painless and can take from 10 minutes to half an hour. The machine analyses the information and develops images of your heart and these images are seen on a monitor. This is referred to as an echocardiogram. Echocardiography can help in the diagnosis of many heart problems including coronary artery disease, previous heart attacks, valve disorders, weakened heart muscle, holes between heart chambers and fluid around the heart (pericardial effusion). A bubble echocardiogram study can be undertaken to diagnose or exclude a hole in the heart. If your doctor is looking for evidence of coronary artery disease he may perform a variation of this test: Exercise echocardiography - a technique used to view how your heart works under stress. It compares how your heart works when stressed by exercise compared with when it is at rest. The ultrasound is undertaken before exercise and immediately after you stop exercising. A standard treadmill is used (see Exercise ECG above). After the test: An Exercise Stress Echo that is clearly negative is reassuring and indicates good cardiac function. The Exercise Test results can be used to direct further investigations and possible treatment.
If your doctor is looking for evidence of coronary artery disease he may perform a variation of this test:
- Exercise echocardiography - a technique used to view how your heart works under stress. It compares how your heart works when stressed by exercise compared with when it is at rest. The ultrasound is undertaken before exercise and immediately after you stop exercising. A standard treadmill is used (see Exercise ECG above).
After the test:
An Exercise Stress Echo that is clearly negative is reassuring and indicates good cardiac function.
The Exercise Test results can be used to direct further investigations and possible treatment.
Patient information: Coronary Artery Calcium Scoring (CACS) is a method to image and quantify calcification within the coronary arteries. It looks for signs of Coronary Artery Disease (CAD) due to the build-up of calcium inside fatty deposits (or atherosclerosis, also called plaque) in the coronary arteries. This technique involves the use of an ECG-gated CT scan and does not require any medicines or intravenous x-ray contrast (dye). With a few breath holds, images of the coronary arteries are taken. Using sophisticated software, the amount of calcium in your coronary arteries from the images is measured, and a score (CAC Score) is calculated from the amount of calcium present. The calcium score is then compared to a reference range for the population of your age and gender, giving a relative risk of developing symptoms of coronary artery disease compared to that of the rest of the population. CACS does not replace functional testing like Exercise Stress Echocardiography, Exercise Tolerance Test or invasive coronary angiography. It stratifies the risk of coronary disease and this can help with the management of coronary artery risk factors.
Patient information: Coronary Artery Calcium Scoring (CACS) is a method to image and quantify calcification within the coronary arteries. It looks for signs of Coronary Artery Disease (CAD) due to the build-up of calcium inside fatty deposits (or atherosclerosis, also called plaque) in the coronary arteries. This technique involves the use of an ECG-gated CT scan and does not require any medicines or intravenous x-ray contrast (dye). With a few breath holds, images of the coronary arteries are taken. Using sophisticated software, the amount of calcium in your coronary arteries from the images is measured, and a score (CAC Score) is calculated from the amount of calcium present. The calcium score is then compared to a reference range for the population of your age and gender, giving a relative risk of developing symptoms of coronary artery disease compared to that of the rest of the population. CACS does not replace functional testing like Exercise Stress Echocardiography, Exercise Tolerance Test or invasive coronary angiography. It stratifies the risk of coronary disease and this can help with the management of coronary artery risk factors.
Patient information:
Coronary Artery Calcium Scoring (CACS) is a method to image and quantify calcification within the coronary arteries. It looks for signs of Coronary Artery Disease (CAD) due to the build-up of calcium inside fatty deposits (or atherosclerosis, also called plaque) in the coronary arteries.
This technique involves the use of an ECG-gated CT scan and does not require any medicines or intravenous x-ray contrast (dye).
With a few breath holds, images of the coronary arteries are taken. Using sophisticated software, the amount of calcium in your coronary arteries from the images is measured, and a score (CAC Score) is calculated from the amount of calcium present. The calcium score is then compared to a reference range for the population of your age and gender, giving a relative risk of developing symptoms of coronary artery disease compared to that of the rest of the population.
CACS does not replace functional testing like Exercise Stress Echocardiography, Exercise Tolerance Test or invasive coronary angiography. It stratifies the risk of coronary disease and this can help with the management of coronary artery risk factors.
Patient information: Event monitoring is a type of electrocardiograph test used to record your heartbeat when you experience symptoms such as palpitations, dizziness or chest pain. This test records your heart rate and rhythm at the time that you have your typical symptoms.
Patient information: Event monitoring is a type of electrocardiograph test used to record your heartbeat when you experience symptoms such as palpitations, dizziness or chest pain. This test records your heart rate and rhythm at the time that you have your typical symptoms.
Patient information:
Event monitoring is a type of electrocardiograph test used to record your heartbeat when you experience symptoms such as palpitations, dizziness or chest pain. This test records your heart rate and rhythm at the time that you have your typical symptoms.
Patient information: A Holter monitor records the heartbeat continuously for 24 hours. This is a small ECG (electrocardiogram) monitor that you wear for 24 hours, and which enables your heart rhythm to be recorded continuously over that time. It is particularly useful if you have had symptoms of palpitations (abnormal awareness of heart beats). You keep a diary of your symptoms and activity during the period of cardiac monitoring. We are able to correlate your symptoms with your heart rhythm at the time that you experience symptoms. Every heart beat that occurs during the 24-hour period is analysed. Such prolonged monitoring may enable the cardiologist to correlate the patient's symptoms with the heart rhythm at the time the symptoms were felt. This correlation is critically important in making a diagnosis in a person complaining of palpitations and dizzy spells. If no symptoms occur during the Holter recording period, more prolonged monitoring may be necessary with other devices such as portable or implantable event recorders. The Holter Monitor Procedure: Four electrodes will be placed on your chest and connected to a Holter recorder (about the size of a matchbox). This recorder fits in a pouch, which straps around the waist, under the clothes. You cannot shower, bathe or use an electric blanket while the recording is being made. After the test: The recording is analysed by a cardiac physiologist in Auckland using a specific computer programme. You are seen in a follow up appointment with Dr Kennedy once the report is available and a copy of the report is sent to your doctor. A letter recommending further investigation or treatment as indicated is then sent to the patient and the referring GP.
Patient information: A Holter monitor records the heartbeat continuously for 24 hours. This is a small ECG (electrocardiogram) monitor that you wear for 24 hours, and which enables your heart rhythm to be recorded continuously over that time. It is particularly useful if you have had symptoms of palpitations (abnormal awareness of heart beats). You keep a diary of your symptoms and activity during the period of cardiac monitoring. We are able to correlate your symptoms with your heart rhythm at the time that you experience symptoms. Every heart beat that occurs during the 24-hour period is analysed. Such prolonged monitoring may enable the cardiologist to correlate the patient's symptoms with the heart rhythm at the time the symptoms were felt. This correlation is critically important in making a diagnosis in a person complaining of palpitations and dizzy spells. If no symptoms occur during the Holter recording period, more prolonged monitoring may be necessary with other devices such as portable or implantable event recorders. The Holter Monitor Procedure: Four electrodes will be placed on your chest and connected to a Holter recorder (about the size of a matchbox). This recorder fits in a pouch, which straps around the waist, under the clothes. You cannot shower, bathe or use an electric blanket while the recording is being made. After the test: The recording is analysed by a cardiac physiologist in Auckland using a specific computer programme. You are seen in a follow up appointment with Dr Kennedy once the report is available and a copy of the report is sent to your doctor. A letter recommending further investigation or treatment as indicated is then sent to the patient and the referring GP.
Patient information:
A Holter monitor records the heartbeat continuously for 24 hours. This is a small ECG (electrocardiogram) monitor that you wear for 24 hours, and which enables your heart rhythm to be recorded continuously over that time. It is particularly useful if you have had symptoms of palpitations (abnormal awareness of heart beats). You keep a diary of your symptoms and activity during the period of cardiac monitoring. We are able to correlate your symptoms with your heart rhythm at the time that you experience symptoms. Every heart beat that occurs during the 24-hour period is analysed. Such prolonged monitoring may enable the cardiologist to correlate the patient's symptoms with the heart rhythm at the time the symptoms were felt. This correlation is critically important in making a diagnosis in a person complaining of palpitations and dizzy spells.
If no symptoms occur during the Holter recording period, more prolonged monitoring may be necessary with other devices such as portable or implantable event recorders.
The Holter Monitor Procedure:
Four electrodes will be placed on your chest and connected to a Holter recorder (about the size of a matchbox). This recorder fits in a pouch, which straps around the waist, under the clothes. You cannot shower, bathe or use an electric blanket while the recording is being made.
After the test:
The recording is analysed by a cardiac physiologist in Auckland using a specific computer programme. You are seen in a follow up appointment with Dr Kennedy once the report is available and a copy of the report is sent to your doctor. A letter recommending further investigation or treatment as indicated is then sent to the patient and the referring GP.
Patient information: High blood pressure (BP) puts an increased load on the heart, brain, kidneys and other organs. If untreated, it can lead to heart attack, heart failure, kidney failure and stroke. High BP usually has no symptoms, so accurate diagnosis by screening is very important. Blood pressure monitoring can be very helpful to determine if a person does have genuinely high BP (it is often higher than normal under stressful conditions, such as visiting the doctor - known as 'white coat hypertension'), or to see how well the BP is controlled by treatment. The ABPM procedure: Ambulatory blood pressure (ABPM) monitors are small, battery-powered units that take blood pressure and heart rate measurements for 24 hours. The unit sits in a pouch strapped around the waist and attaches via rubber tubing to an inflatable cuff, which is wrapped around the upper arm. An ambulatory monitor takes about 40 BP readings over 24 hours. Your blood pressure is recorded half hourly during the day and hourly at night. The machine can show the maximum, minimum and average BP at different times of the day. The BP monitor saves the measurements of your blood pressure that have been captured in the 24 hours of the recording. The blood pressure measurements are then downloaded and analysed. This can be very helpful in tailoring the best type, and the timing of BP treatment. The recorder inflates the cuff to measure the blood pressure then deflates the cuff again. The cuff can feel quite tight around the arm when inflated, and can briefly be uncomfortable. My nurse will explain the procedure and fit the monitor, which takes approximately 20 - 30 minutes. No special preparations are necessary for the test, but it is sensible to wear a loose fitting top or jacket if possible. A diary will need to be filled in, so that BP changes can be correlated with activity during the 24 hour period. Removing the monitor the next day takes only a few minutes. It is not possible to shower or bathe whilst wearing the unit. After the test: A report is prepared showing the individual blood pressures, as well as the average, maximum and minimum BP during the day and at night. A copy of the report is sent to the referring doctor (and to the patient themselves on request). This is usually done within 2-4 days of the test being completed.
Patient information: High blood pressure (BP) puts an increased load on the heart, brain, kidneys and other organs. If untreated, it can lead to heart attack, heart failure, kidney failure and stroke. High BP usually has no symptoms, so accurate diagnosis by screening is very important. Blood pressure monitoring can be very helpful to determine if a person does have genuinely high BP (it is often higher than normal under stressful conditions, such as visiting the doctor - known as 'white coat hypertension'), or to see how well the BP is controlled by treatment. The ABPM procedure: Ambulatory blood pressure (ABPM) monitors are small, battery-powered units that take blood pressure and heart rate measurements for 24 hours. The unit sits in a pouch strapped around the waist and attaches via rubber tubing to an inflatable cuff, which is wrapped around the upper arm. An ambulatory monitor takes about 40 BP readings over 24 hours. Your blood pressure is recorded half hourly during the day and hourly at night. The machine can show the maximum, minimum and average BP at different times of the day. The BP monitor saves the measurements of your blood pressure that have been captured in the 24 hours of the recording. The blood pressure measurements are then downloaded and analysed. This can be very helpful in tailoring the best type, and the timing of BP treatment. The recorder inflates the cuff to measure the blood pressure then deflates the cuff again. The cuff can feel quite tight around the arm when inflated, and can briefly be uncomfortable. My nurse will explain the procedure and fit the monitor, which takes approximately 20 - 30 minutes. No special preparations are necessary for the test, but it is sensible to wear a loose fitting top or jacket if possible. A diary will need to be filled in, so that BP changes can be correlated with activity during the 24 hour period. Removing the monitor the next day takes only a few minutes. It is not possible to shower or bathe whilst wearing the unit. After the test: A report is prepared showing the individual blood pressures, as well as the average, maximum and minimum BP during the day and at night. A copy of the report is sent to the referring doctor (and to the patient themselves on request). This is usually done within 2-4 days of the test being completed.
Patient information:
High blood pressure (BP) puts an increased load on the heart, brain, kidneys and other organs. If untreated, it can lead to heart attack, heart failure, kidney failure and stroke. High BP usually has no symptoms, so accurate diagnosis by screening is very important.
Blood pressure monitoring can be very helpful to determine if a person does have genuinely high BP (it is often higher than normal under stressful conditions, such as visiting the doctor - known as 'white coat hypertension'), or to see how well the BP is controlled by treatment.
The ABPM procedure:
Ambulatory blood pressure (ABPM) monitors are small, battery-powered units that take blood pressure and heart rate measurements for 24 hours. The unit sits in a pouch strapped around the waist and attaches via rubber tubing to an inflatable cuff, which is wrapped around the upper arm. An ambulatory monitor takes about 40 BP readings over 24 hours. Your blood pressure is recorded half hourly during the day and hourly at night. The machine can show the maximum, minimum and average BP at different times of the day. The BP monitor saves the measurements of your blood pressure that have been captured in the 24 hours of the recording. The blood pressure measurements are then downloaded and analysed. This can be very helpful in tailoring the best type, and the timing of BP treatment. The recorder inflates the cuff to measure the blood pressure then deflates the cuff again. The cuff can feel quite tight around the arm when inflated, and can briefly be uncomfortable.
My nurse will explain the procedure and fit the monitor, which takes approximately 20 - 30 minutes. No special preparations are necessary for the test, but it is sensible to wear a loose fitting top or jacket if possible. A diary will need to be filled in, so that BP changes can be correlated with activity during the 24 hour period. Removing the monitor the next day takes only a few minutes. It is not possible to shower or bathe whilst wearing the unit.
After the test:
A report is prepared showing the individual blood pressures, as well as the average, maximum and minimum BP during the day and at night. A copy of the report is sent to the referring doctor (and to the patient themselves on request). This is usually done within 2-4 days of the test being completed.
Patient information: Electrical cardioversion is a procedure used to correct rhythm abnormalities of the heart, in which a small electric shock is used to "jolt" the heart back into a normal rhythm. The procedure is usually undertaken for the common rhythm disturbances, atrial fibrillation and atrial flutter. If the abnormal rhythm has been present for more than 48 hours, the patient will usually be treated with Dabigatran or Warfarin (an anticoagulant, or "blood thinner") for at least 3 weeks prior to a cardioversion. This is to ensure that there is no blood clot in the heart, which could be released into the circulation by the cardioversion causing a significant problem, such as a stroke. Sometimes a transoesophageal echo may be performed immediately before a cardioversion to exclude the presence of any blood clot inside the heart. Medicines are often given to hold the rhythm stable when there is a successful cardioversion. Blood thinning with Dabigatran or Warfarin is required to reduce the risk of clotting and stroke for an interval both before and following the procedure. Electrical cardioversion has a high immediate success rate, and is a low risk procedure. The procedure is performed under a short general anaesthetic, and the patient must fast for 4 - 6 hours before the procedure. The shock is delivered through electrode pads placed on the chest and back. Up to 3 shocks may be given in an attempt to restore the heart's natural rhythm (sinus rhythm). After the procedure: Following cardioversion the patient is monitored for approximately one hour, and should not drive for 24 hours. A report will be sent to the referring doctor or GP, and the cardiologist performing the procedure will explain ongoing treatment and medication to you. If you have been on Dabigatran or Warfarin, it is important to continue this, usually for at least 4 weeks after the cardioversion. This will be discussed at your follow-up visit in 4 weeks' time. On occasions cardioversion can be repeated if the rhythm disturbance recurs.
Patient information: Electrical cardioversion is a procedure used to correct rhythm abnormalities of the heart, in which a small electric shock is used to "jolt" the heart back into a normal rhythm. The procedure is usually undertaken for the common rhythm disturbances, atrial fibrillation and atrial flutter. If the abnormal rhythm has been present for more than 48 hours, the patient will usually be treated with Dabigatran or Warfarin (an anticoagulant, or "blood thinner") for at least 3 weeks prior to a cardioversion. This is to ensure that there is no blood clot in the heart, which could be released into the circulation by the cardioversion causing a significant problem, such as a stroke. Sometimes a transoesophageal echo may be performed immediately before a cardioversion to exclude the presence of any blood clot inside the heart. Medicines are often given to hold the rhythm stable when there is a successful cardioversion. Blood thinning with Dabigatran or Warfarin is required to reduce the risk of clotting and stroke for an interval both before and following the procedure. Electrical cardioversion has a high immediate success rate, and is a low risk procedure. The procedure is performed under a short general anaesthetic, and the patient must fast for 4 - 6 hours before the procedure. The shock is delivered through electrode pads placed on the chest and back. Up to 3 shocks may be given in an attempt to restore the heart's natural rhythm (sinus rhythm). After the procedure: Following cardioversion the patient is monitored for approximately one hour, and should not drive for 24 hours. A report will be sent to the referring doctor or GP, and the cardiologist performing the procedure will explain ongoing treatment and medication to you. If you have been on Dabigatran or Warfarin, it is important to continue this, usually for at least 4 weeks after the cardioversion. This will be discussed at your follow-up visit in 4 weeks' time. On occasions cardioversion can be repeated if the rhythm disturbance recurs.
Patient information:
Electrical cardioversion is a procedure used to correct rhythm abnormalities of the heart, in which a small electric shock is used to "jolt" the heart back into a normal rhythm. The procedure is usually undertaken for the common rhythm disturbances, atrial fibrillation and atrial flutter. If the abnormal rhythm has been present for more than 48 hours, the patient will usually be treated with Dabigatran or Warfarin (an anticoagulant, or "blood thinner") for at least 3 weeks prior to a cardioversion. This is to ensure that there is no blood clot in the heart, which could be released into the circulation by the cardioversion causing a significant problem, such as a stroke. Sometimes a transoesophageal echo may be performed immediately before a cardioversion to exclude the presence of any blood clot inside the heart.
Medicines are often given to hold the rhythm stable when there is a successful cardioversion. Blood thinning with Dabigatran or Warfarin is required to reduce the risk of clotting and stroke for an interval both before and following the procedure. Electrical cardioversion has a high immediate success rate, and is a low risk procedure.
The procedure is performed under a short general anaesthetic, and the patient must fast for 4 - 6 hours before the procedure. The shock is delivered through electrode pads placed on the chest and back. Up to 3 shocks may be given in an attempt to restore the heart's natural rhythm (sinus rhythm).
After the procedure:
Following cardioversion the patient is monitored for approximately one hour, and should not drive for 24 hours. A report will be sent to the referring doctor or GP, and the cardiologist performing the procedure will explain ongoing treatment and medication to you. If you have been on Dabigatran or Warfarin, it is important to continue this, usually for at least 4 weeks after the cardioversion. This will be discussed at your follow-up visit in 4 weeks' time.
On occasions cardioversion can be repeated if the rhythm disturbance recurs.
Patient information: This is a procedure which allows Dr Kennedy to see inside your oesophagus, stomach, and the first part of the small intestine (duodenum) allowing direct examination of the lining. This is undertaken by Dr Kennedy at Kensington Hospital. Dr Kennedy is a Southern Cross Affiliated Provider for gastroscopy. What to expect You will be offered intravenous sedatives (medicine that will make you drowsy, though not a general anaesthetic) and this will dim any recollection of the event. The throat is sprayed with local anaesthetic so you don’t feel the gastroscope. During the test the gastroscope will be passed through the mouth, down the back of your throat. The gastroscope is a plastic-coated tube about as thin as a ballpoint pen and is soft and flexible. It has a tiny camera attached that sends images to a viewing screen. If Dr Kennedy sees any abnormalities he can take a biopsy (a small piece of tissue) to send to the laboratory for testing. This is not a painful procedure and will be performed at the day stay unit in a theatre suite (operating room) at Kensington Hospital by Dr Kennedy, with nurses assisting. Complications from this procedure are very rare, but can occur. They include: bleeding after a biopsy, if performed an allergic reaction to the sedative or throat spray or complications from the sedation perforation (tearing) of the oesophagus or stomach with the instrument (this is a serious but extremely rare complication) Before the procedure: You will be asked not to eat or drink anything for 6 hours before the gastroscopy. An early small breakfast is possible if you are on an afternoon procedure list. After the procedure: Dr Kennedy wishes to speak about the findings with someone else as you will be sedated and will have either no or only minimal recollection of conversations after the procedure. You will stay in the day stay unit until the sedation has worn off, which usually takes 1-2 hours. You will be given something to eat and drink before you go home. You must not drive until the following day as you have received sedation. You need someone to drive you home and keep an eye on you until the following day. Prearrangements for overnight admission can be made if you cannot be driven home. If biopsies are taken these will be sent for histological (microscopic) analysis and results are usually available within 1 week. A report and copy of these biopsy results and the gastroscopy report and photos are sent to your GP. In some cases you will need to be followed up in the clinic with Dr Kennedy or you may need a follow-up gastroscopy after an interval, depending on the nature of your problem.
Patient information: This is a procedure which allows Dr Kennedy to see inside your oesophagus, stomach, and the first part of the small intestine (duodenum) allowing direct examination of the lining. This is undertaken by Dr Kennedy at Kensington Hospital. Dr Kennedy is a Southern Cross Affiliated Provider for gastroscopy. What to expect You will be offered intravenous sedatives (medicine that will make you drowsy, though not a general anaesthetic) and this will dim any recollection of the event. The throat is sprayed with local anaesthetic so you don’t feel the gastroscope. During the test the gastroscope will be passed through the mouth, down the back of your throat. The gastroscope is a plastic-coated tube about as thin as a ballpoint pen and is soft and flexible. It has a tiny camera attached that sends images to a viewing screen. If Dr Kennedy sees any abnormalities he can take a biopsy (a small piece of tissue) to send to the laboratory for testing. This is not a painful procedure and will be performed at the day stay unit in a theatre suite (operating room) at Kensington Hospital by Dr Kennedy, with nurses assisting. Complications from this procedure are very rare, but can occur. They include: bleeding after a biopsy, if performed an allergic reaction to the sedative or throat spray or complications from the sedation perforation (tearing) of the oesophagus or stomach with the instrument (this is a serious but extremely rare complication) Before the procedure: You will be asked not to eat or drink anything for 6 hours before the gastroscopy. An early small breakfast is possible if you are on an afternoon procedure list. After the procedure: Dr Kennedy wishes to speak about the findings with someone else as you will be sedated and will have either no or only minimal recollection of conversations after the procedure. You will stay in the day stay unit until the sedation has worn off, which usually takes 1-2 hours. You will be given something to eat and drink before you go home. You must not drive until the following day as you have received sedation. You need someone to drive you home and keep an eye on you until the following day. Prearrangements for overnight admission can be made if you cannot be driven home. If biopsies are taken these will be sent for histological (microscopic) analysis and results are usually available within 1 week. A report and copy of these biopsy results and the gastroscopy report and photos are sent to your GP. In some cases you will need to be followed up in the clinic with Dr Kennedy or you may need a follow-up gastroscopy after an interval, depending on the nature of your problem.
Patient information:
This is a procedure which allows Dr Kennedy to see inside your oesophagus, stomach, and the first part of the small intestine (duodenum) allowing direct examination of the lining. This is undertaken by Dr Kennedy at Kensington Hospital. Dr Kennedy is a Southern Cross Affiliated Provider for gastroscopy.
What to expect
You will be offered intravenous sedatives (medicine that will make you drowsy, though not a general anaesthetic) and this will dim any recollection of the event. The throat is sprayed with local anaesthetic so you don’t feel the gastroscope. During the test the gastroscope will be passed through the mouth, down the back of your throat. The gastroscope is a plastic-coated tube about as thin as a ballpoint pen and is soft and flexible. It has a tiny camera attached that sends images to a viewing screen. If Dr Kennedy sees any abnormalities he can take a biopsy (a small piece of tissue) to send to the laboratory for testing. This is not a painful procedure and will be performed at the day stay unit in a theatre suite (operating room) at Kensington Hospital by Dr Kennedy, with nurses assisting.
Complications from this procedure are very rare, but can occur. They include:
- bleeding after a biopsy, if performed
- an allergic reaction to the sedative or throat spray or complications from the sedation
- perforation (tearing) of the oesophagus or stomach with the instrument (this is a serious but extremely rare complication)
Before the procedure: You will be asked not to eat or drink anything for 6 hours before the gastroscopy. An early small breakfast is possible if you are on an afternoon procedure list.
After the procedure: Dr Kennedy wishes to speak about the findings with someone else as you will be sedated and will have either no or only minimal recollection of conversations after the procedure. You will stay in the day stay unit until the sedation has worn off, which usually takes 1-2 hours. You will be given something to eat and drink before you go home. You must not drive until the following day as you have received sedation. You need someone to drive you home and keep an eye on you until the following day. Prearrangements for overnight admission can be made if you cannot be driven home.
If biopsies are taken these will be sent for histological (microscopic) analysis and results are usually available within 1 week. A report and copy of these biopsy results and the gastroscopy report and photos are sent to your GP. In some cases you will need to be followed up in the clinic with Dr Kennedy or you may need a follow-up gastroscopy after an interval, depending on the nature of your problem.
Patient information: The best way to establish what type of liver disease is present and the extent and stage of the disease, is with a liver biopsy. Before Dr Kennedy does this procedure, he will check whether or not you are at increased risk of bleeding by requesting clotting blood tests. Aspirin, Clopidogrel, Ticagrelor, non-steroidal anti-inflammatories, Warfarin, Dabigatran, omega-3 and other blood thinners will need to be withheld for up to 1 week prior to the liver biopsy. After ultrasound marking, good local anaesthesia and analgesia, the biopsy is performed by inserting a skinny needle into the liver through the skin, and taking a small sample of liver tissue. Examination of the liver biopsy sample under the microscope can demonstrate the presence of inflammation, and the degree of fibrosis or cirrhosis (scarring) and often what type of underlying liver disease is present. After the procedure: Following the procedure, you will need to be monitored for four hours before you are able to be discharged to go home. Paracetamol can be used as analgesia. You will be seen in the clinic a week after the biopsy to review the results and discuss the management plan.
Patient information: The best way to establish what type of liver disease is present and the extent and stage of the disease, is with a liver biopsy. Before Dr Kennedy does this procedure, he will check whether or not you are at increased risk of bleeding by requesting clotting blood tests. Aspirin, Clopidogrel, Ticagrelor, non-steroidal anti-inflammatories, Warfarin, Dabigatran, omega-3 and other blood thinners will need to be withheld for up to 1 week prior to the liver biopsy. After ultrasound marking, good local anaesthesia and analgesia, the biopsy is performed by inserting a skinny needle into the liver through the skin, and taking a small sample of liver tissue. Examination of the liver biopsy sample under the microscope can demonstrate the presence of inflammation, and the degree of fibrosis or cirrhosis (scarring) and often what type of underlying liver disease is present. After the procedure: Following the procedure, you will need to be monitored for four hours before you are able to be discharged to go home. Paracetamol can be used as analgesia. You will be seen in the clinic a week after the biopsy to review the results and discuss the management plan.
Patient information:
The best way to establish what type of liver disease is present and the extent and stage of the disease, is with a liver biopsy.
Before Dr Kennedy does this procedure, he will check whether or not you are at increased risk of bleeding by requesting clotting blood tests. Aspirin, Clopidogrel, Ticagrelor, non-steroidal anti-inflammatories, Warfarin, Dabigatran, omega-3 and other blood thinners will need to be withheld for up to 1 week prior to the liver biopsy.
After ultrasound marking, good local anaesthesia and analgesia, the biopsy is performed by inserting a skinny needle into the liver through the skin, and taking a small sample of liver tissue. Examination of the liver biopsy sample under the microscope can demonstrate the presence of inflammation, and the degree of fibrosis or cirrhosis (scarring) and often what type of underlying liver disease is present.
After the procedure:
Following the procedure, you will need to be monitored for four hours before you are able to be discharged to go home. Paracetamol can be used as analgesia.
You will be seen in the clinic a week after the biopsy to review the results and discuss the management plan.
Patient information: Dr Kennedy can arrange for this procedure in Auckland or Whangarei. Before and during the procedure: You will be asked not to eat anything for 6 hours before and not to take any of your medications on the day of the procedure. Aspirin, Clopidogrel, Ticagrelor, non-steroidal anti-inflammatories, omega-3 and Warfarin, Dabigatran and other blood thinners will need to be withheld up to 1 week prior to the bronchoscopy. Bronchoscopy is usually undertaken under combined local anaesthetic spray and sedation. You will be given medicine to make you sleepy and relaxed. Oxygen is given during the procedure and the oxygen level in the blood and heart rate are monitored. Nursing staff help before, during and after the procedure. During this test a thin fibre optic tube is passed through the mouth and over your tongue, through the vocal cords and into your breathing tubes. This allows a good view of the bronchial tubes and the ability to take a biopsy (remove cells or tissue) to see if a diagnosis of your condition can be made. Both sides are carefully inspected. If tissue that looks unusual is seen, biopsies are taken with a fine set of forceps which fit inside the bronchoscope. Washings are often taken, and they are sent for cytology and/or culture for various organisms, when appropriate. After the procedure: You will stay in the day stay unit until the sedation has worn off, which usually takes 1 - 1.5 hours. Eating or drinking before the anaesthetic has worn off can result in food or fluids going down into the breathing tubes instead of the swallowing tube (or oesophagus). You will be given something to eat and drink before you go home. If you have been sedated, you will not be able to drive until the following day. You need someone to drive you home and keep an eye on you until the following day. If biopsies are taken, these will be sent for analysis and results are usually available within 1 week. A report and copy of these biopsy results and the bronchoscopy report are sent to your GP. You will need to be followed up in the clinic with Dr Kennedy 1-2 weeks later, to discuss the results of the bronchoscopy.
Patient information: Dr Kennedy can arrange for this procedure in Auckland or Whangarei. Before and during the procedure: You will be asked not to eat anything for 6 hours before and not to take any of your medications on the day of the procedure. Aspirin, Clopidogrel, Ticagrelor, non-steroidal anti-inflammatories, omega-3 and Warfarin, Dabigatran and other blood thinners will need to be withheld up to 1 week prior to the bronchoscopy. Bronchoscopy is usually undertaken under combined local anaesthetic spray and sedation. You will be given medicine to make you sleepy and relaxed. Oxygen is given during the procedure and the oxygen level in the blood and heart rate are monitored. Nursing staff help before, during and after the procedure. During this test a thin fibre optic tube is passed through the mouth and over your tongue, through the vocal cords and into your breathing tubes. This allows a good view of the bronchial tubes and the ability to take a biopsy (remove cells or tissue) to see if a diagnosis of your condition can be made. Both sides are carefully inspected. If tissue that looks unusual is seen, biopsies are taken with a fine set of forceps which fit inside the bronchoscope. Washings are often taken, and they are sent for cytology and/or culture for various organisms, when appropriate. After the procedure: You will stay in the day stay unit until the sedation has worn off, which usually takes 1 - 1.5 hours. Eating or drinking before the anaesthetic has worn off can result in food or fluids going down into the breathing tubes instead of the swallowing tube (or oesophagus). You will be given something to eat and drink before you go home. If you have been sedated, you will not be able to drive until the following day. You need someone to drive you home and keep an eye on you until the following day. If biopsies are taken, these will be sent for analysis and results are usually available within 1 week. A report and copy of these biopsy results and the bronchoscopy report are sent to your GP. You will need to be followed up in the clinic with Dr Kennedy 1-2 weeks later, to discuss the results of the bronchoscopy.
Patient information:
Dr Kennedy can arrange for this procedure in Auckland or Whangarei.
Before and during the procedure:
You will be asked not to eat anything for 6 hours before and not to take any of your medications on the day of the procedure. Aspirin, Clopidogrel, Ticagrelor, non-steroidal anti-inflammatories, omega-3 and Warfarin, Dabigatran and other blood thinners will need to be withheld up to 1 week prior to the bronchoscopy.
Bronchoscopy is usually undertaken under combined local anaesthetic spray and sedation. You will be given medicine to make you sleepy and relaxed. Oxygen is given during the procedure and the oxygen level in the blood and heart rate are monitored. Nursing staff help before, during and after the procedure.
During this test a thin fibre optic tube is passed through the mouth and over your tongue, through the vocal cords and into your breathing tubes. This allows a good view of the bronchial tubes and the ability to take a biopsy (remove cells or tissue) to see if a diagnosis of your condition can be made. Both sides are carefully inspected. If tissue that looks unusual is seen, biopsies are taken with a fine set of forceps which fit inside the bronchoscope. Washings are often taken, and they are sent for cytology and/or culture for various organisms, when appropriate.
After the procedure:
You will stay in the day stay unit until the sedation has worn off, which usually takes 1 - 1.5 hours. Eating or drinking before the anaesthetic has worn off can result in food or fluids going down into the breathing tubes instead of the swallowing tube (or oesophagus). You will be given something to eat and drink before you go home. If you have been sedated, you will not be able to drive until the following day. You need someone to drive you home and keep an eye on you until the following day.
If biopsies are taken, these will be sent for analysis and results are usually available within 1 week. A report and copy of these biopsy results and the bronchoscopy report are sent to your GP. You will need to be followed up in the clinic with Dr Kennedy 1-2 weeks later, to discuss the results of the bronchoscopy.
Patient information: Spirometry is a test which measures the volume of air with which your lungs can be filled and the rate that you can empty your lungs. It can be used to diagnose problems of breathing and airflow limitation and to monitor the usefulness of treatment. In order to do spirometry, you take a deep breath in and then blow out as hard as you can into a hollow tube attached to a spirometer machine for 6 or more seconds. You will be asked to do the test at least 3 times to ensure reliability of the test and to capture your best result. Spirometry measures the volume of air expelled from the lungs in the first second and the total amount exhaled by the person doing the test. It also gives a measure of flow through small airways (or bronchioles). Restriction and obstruction are different patterns that spirometry can detect, as well as showing the severity of the abnormalities. I perform this type of test routinely in my office on people who are breathless or where asthma, emphysema or COPD are suspected. Your results are compared with a normal non-smoker of your age, height and gender.
Patient information: Spirometry is a test which measures the volume of air with which your lungs can be filled and the rate that you can empty your lungs. It can be used to diagnose problems of breathing and airflow limitation and to monitor the usefulness of treatment. In order to do spirometry, you take a deep breath in and then blow out as hard as you can into a hollow tube attached to a spirometer machine for 6 or more seconds. You will be asked to do the test at least 3 times to ensure reliability of the test and to capture your best result. Spirometry measures the volume of air expelled from the lungs in the first second and the total amount exhaled by the person doing the test. It also gives a measure of flow through small airways (or bronchioles). Restriction and obstruction are different patterns that spirometry can detect, as well as showing the severity of the abnormalities. I perform this type of test routinely in my office on people who are breathless or where asthma, emphysema or COPD are suspected. Your results are compared with a normal non-smoker of your age, height and gender.
Patient information:
Spirometry is a test which measures the volume of air with which your lungs can be filled and the rate that you can empty your lungs. It can be used to diagnose problems of breathing and airflow limitation and to monitor the usefulness of treatment.
In order to do spirometry, you take a deep breath in and then blow out as hard as you can into a hollow tube attached to a spirometer machine for 6 or more seconds. You will be asked to do the test at least 3 times to ensure reliability of the test and to capture your best result.
Spirometry measures the volume of air expelled from the lungs in the first second and the total amount exhaled by the person doing the test. It also gives a measure of flow through small airways (or bronchioles). Restriction and obstruction are different patterns that spirometry can detect, as well as showing the severity of the abnormalities.
I perform this type of test routinely in my office on people who are breathless or where asthma, emphysema or COPD are suspected.
Your results are compared with a normal non-smoker of your age, height and gender.
Patient information: This testing is undertaken with an experienced Lung Function Technician. You may be advised to have lung function tests to find out how much air moves in and out as you breathe and to measure the diffusion of gas. Lung function is often measured in a closed see-through cubicle, in a process called plethysmography. Lung function tests are sometimes done before and after taking a medication known as a bronchodilator (asthma reliever medication) to open your airways and look for signs of improvement. 'Detailed lung function tests' are performed in a lung function laboratory. These tests include the spirometric values, but the total volume of the lungs and various fractions of lung volumes are also measured. The ability of oxygen to diffuse into the blood through the alveolar walls is measured by the 'diffusing capacity', which is low in people with emphysema, interstitial lung disease and pulmonary hypertension. Your results are compared with a normal non-smoker of your age, height and gender. After the procedure: You will be seen by Dr Kennedy in clinic for a follow-up appointment to discuss the results and their significance. A copy of your results will be sent to your GP.
Patient information: This testing is undertaken with an experienced Lung Function Technician. You may be advised to have lung function tests to find out how much air moves in and out as you breathe and to measure the diffusion of gas. Lung function is often measured in a closed see-through cubicle, in a process called plethysmography. Lung function tests are sometimes done before and after taking a medication known as a bronchodilator (asthma reliever medication) to open your airways and look for signs of improvement. 'Detailed lung function tests' are performed in a lung function laboratory. These tests include the spirometric values, but the total volume of the lungs and various fractions of lung volumes are also measured. The ability of oxygen to diffuse into the blood through the alveolar walls is measured by the 'diffusing capacity', which is low in people with emphysema, interstitial lung disease and pulmonary hypertension. Your results are compared with a normal non-smoker of your age, height and gender. After the procedure: You will be seen by Dr Kennedy in clinic for a follow-up appointment to discuss the results and their significance. A copy of your results will be sent to your GP.
Patient information:
This testing is undertaken with an experienced Lung Function Technician.
You may be advised to have lung function tests to find out how much air moves in and out as you breathe and to measure the diffusion of gas. Lung function is often measured in a closed see-through cubicle, in a process called plethysmography. Lung function tests are sometimes done before and after taking a medication known as a bronchodilator (asthma reliever medication) to open your airways and look for signs of improvement.
'Detailed lung function tests' are performed in a lung function laboratory. These tests include the spirometric values, but the total volume of the lungs and various fractions of lung volumes are also measured. The ability of oxygen to diffuse into the blood through the alveolar walls is measured by the 'diffusing capacity', which is low in people with emphysema, interstitial lung disease and pulmonary hypertension.
Your results are compared with a normal non-smoker of your age, height and gender.
After the procedure:
You will be seen by Dr Kennedy in clinic for a follow-up appointment to discuss the results and their significance. A copy of your results will be sent to your GP.
Patient information: Pleural aspiration and biopsy are most often undertaken to diagnose the cause for pleural fluid or pleural mass/thickening. These procedures are usually undertaken under local anaesthesia after ultrasound marking, or under CT guidance. Pleural aspiration and biopsy are performed to try and diagnose the cause of the problem such as inflammation, infection, tuberculosis or cancer. Pleural aspiration and pleural biopsy: These procedures can be done in different ways. A surgeon can perform them, usually thoracoscopically (i.e. 'key hole' surgery in which thin, rigid telescopes to which biopsy forceps or other instruments can be attached, are inserted through the chest wall). Thoracoscopy requires a general anaesthetic and one or more days in hospital. Pleural aspiration and biopsy are usually undertaken under local anaesthetic and sedation, using a special needle which is much finer than the instruments a surgeon uses. Afterwards the patient has a chest X-ray and then returns home. The best site for inserting the special needle is located beforehand by ultrasound (i.e. bouncing sound waves through the chest wall), confirming there is fluid at that site. Local anaesthetic is injected under the skin and then into the muscle at that site, before inserting the needle through which biopsies and fluid can be collected. The procedure can take anything from 20 - 60 minutes, depending on how much fluid has to be removed. The aspiration and biopsy site are closed with a suture (i.e. a stitch) that needs to be removed about 5 days later by your GP. Is pleural aspiration or pleural biopsy painful? This depends to a large extent on the skill of the person doing the procedure. Performed by an expert, they should be pain-free or almost pain-free. If there is discomfort I will always do my best to minimise it. Care is needed with very large pleural effusions (e.g. where there is more than 1.5 litres of fluid) or the effusion has been present for a long time. Rapid removal of fluid can cause pain or make breathing worse. In these situations it is sometimes better to insert a pleural tube/catheter and drain the fluid slowly over several hours, in hospital. The doctor removing pleural fluid needs experience and patience. Why is a pleural aspiration needed? There are three main reasons: Firstly, to diagnose the cause of the pleural effusion. Secondly, to give relief from the breathlessness caused by a large pleural effusion. Lastly, to see whether, following the removal of most of the fluid, the lung has fully re-expanded and is sitting adjacent to the chest wall and the mediastinum (i.e. the tissues in the centre of the chest). This information is needed in the context of pleural effusion caused by a cancer. Sometimes recurrent pleural effusion caused by cancer can be eliminated by doing a 'pleurodesis'. This involves putting a chemical or talc into the pleural space (by a surgeon). However, this only works if the lung can fully re-expand against the chest wall. If the lung can re-expand, pleurodesis can be done. After the procedure: The results usually take a week or more to return. When the results are available, they are reviewed with you and management plan options are discussed in Dr Kennedy's rooms.
Patient information: Pleural aspiration and biopsy are most often undertaken to diagnose the cause for pleural fluid or pleural mass/thickening. These procedures are usually undertaken under local anaesthesia after ultrasound marking, or under CT guidance. Pleural aspiration and biopsy are performed to try and diagnose the cause of the problem such as inflammation, infection, tuberculosis or cancer. Pleural aspiration and pleural biopsy: These procedures can be done in different ways. A surgeon can perform them, usually thoracoscopically (i.e. 'key hole' surgery in which thin, rigid telescopes to which biopsy forceps or other instruments can be attached, are inserted through the chest wall). Thoracoscopy requires a general anaesthetic and one or more days in hospital. Pleural aspiration and biopsy are usually undertaken under local anaesthetic and sedation, using a special needle which is much finer than the instruments a surgeon uses. Afterwards the patient has a chest X-ray and then returns home. The best site for inserting the special needle is located beforehand by ultrasound (i.e. bouncing sound waves through the chest wall), confirming there is fluid at that site. Local anaesthetic is injected under the skin and then into the muscle at that site, before inserting the needle through which biopsies and fluid can be collected. The procedure can take anything from 20 - 60 minutes, depending on how much fluid has to be removed. The aspiration and biopsy site are closed with a suture (i.e. a stitch) that needs to be removed about 5 days later by your GP. Is pleural aspiration or pleural biopsy painful? This depends to a large extent on the skill of the person doing the procedure. Performed by an expert, they should be pain-free or almost pain-free. If there is discomfort I will always do my best to minimise it. Care is needed with very large pleural effusions (e.g. where there is more than 1.5 litres of fluid) or the effusion has been present for a long time. Rapid removal of fluid can cause pain or make breathing worse. In these situations it is sometimes better to insert a pleural tube/catheter and drain the fluid slowly over several hours, in hospital. The doctor removing pleural fluid needs experience and patience. Why is a pleural aspiration needed? There are three main reasons: Firstly, to diagnose the cause of the pleural effusion. Secondly, to give relief from the breathlessness caused by a large pleural effusion. Lastly, to see whether, following the removal of most of the fluid, the lung has fully re-expanded and is sitting adjacent to the chest wall and the mediastinum (i.e. the tissues in the centre of the chest). This information is needed in the context of pleural effusion caused by a cancer. Sometimes recurrent pleural effusion caused by cancer can be eliminated by doing a 'pleurodesis'. This involves putting a chemical or talc into the pleural space (by a surgeon). However, this only works if the lung can fully re-expand against the chest wall. If the lung can re-expand, pleurodesis can be done. After the procedure: The results usually take a week or more to return. When the results are available, they are reviewed with you and management plan options are discussed in Dr Kennedy's rooms.
Patient information:
Pleural aspiration and biopsy are most often undertaken to diagnose the cause for pleural fluid or pleural mass/thickening. These procedures are usually undertaken under local anaesthesia after ultrasound marking, or under CT guidance. Pleural aspiration and biopsy are performed to try and diagnose the cause of the problem such as inflammation, infection, tuberculosis or cancer.
Pleural aspiration and pleural biopsy:
These procedures can be done in different ways. A surgeon can perform them, usually thoracoscopically (i.e. 'key hole' surgery in which thin, rigid telescopes to which biopsy forceps or other instruments can be attached, are inserted through the chest wall). Thoracoscopy requires a general anaesthetic and one or more days in hospital.
Pleural aspiration and biopsy are usually undertaken under local anaesthetic and sedation, using a special needle which is much finer than the instruments a surgeon uses. Afterwards the patient has a chest X-ray and then returns home.
The best site for inserting the special needle is located beforehand by ultrasound (i.e. bouncing sound waves through the chest wall), confirming there is fluid at that site. Local anaesthetic is injected under the skin and then into the muscle at that site, before inserting the needle through which biopsies and fluid can be collected.
The procedure can take anything from 20 - 60 minutes, depending on how much fluid has to be removed. The aspiration and biopsy site are closed with a suture (i.e. a stitch) that needs to be removed about 5 days later by your GP.
Is pleural aspiration or pleural biopsy painful?
This depends to a large extent on the skill of the person doing the procedure. Performed by an expert, they should be pain-free or almost pain-free. If there is discomfort I will always do my best to minimise it.
Care is needed with very large pleural effusions (e.g. where there is more than 1.5 litres of fluid) or the effusion has been present for a long time. Rapid removal of fluid can cause pain or make breathing worse. In these situations it is sometimes better to insert a pleural tube/catheter and drain the fluid slowly over several hours, in hospital.
The doctor removing pleural fluid needs experience and patience.
Why is a pleural aspiration needed?
There are three main reasons:
- Firstly, to diagnose the cause of the pleural effusion.
- Secondly, to give relief from the breathlessness caused by a large pleural effusion.
- Lastly, to see whether, following the removal of most of the fluid, the lung has fully re-expanded and is sitting adjacent to the chest wall and the mediastinum (i.e. the tissues in the centre of the chest). This information is needed in the context of pleural effusion caused by a cancer. Sometimes recurrent pleural effusion caused by cancer can be eliminated by doing a 'pleurodesis'. This involves putting a chemical or talc into the pleural space (by a surgeon). However, this only works if the lung can fully re-expand against the chest wall. If the lung can re-expand, pleurodesis can be done.
After the procedure:
The results usually take a week or more to return. When the results are available, they are reviewed with you and management plan options are discussed in Dr Kennedy's rooms.
Patient information: This refers to narrowing of the arteries that supply blood to the heart muscle. The heart, like all other organs in the body, needs a constant supply of oxygen and energy. Narrowed arteries are unable to keep up with the demand needed to supply the heart muscle with blood and oxygen. A coronary artery narrowing (stenosis) or obstruction can cause damage to the heart muscle. The most common symptom of this problem is chest pain or tightness that occurs when you exert yourself (angina). Typical angina chest pain is a heavy sensation in your chest associated with shortness of breath. The pain sometimes radiates to your arms and can make you feel nauseated, breathless, dizzy or sweaty. Not everybody experiences the same sensation and any one of those symptoms can represent angina. If your GP thinks you may have angina, they will refer you for an assessment to plan treatment. Heart Attack (Myocardial Infarction) If an attack of chest pain lasts for more than 20 minutes, then you may be having a heart attack. This is when a piece of the heart muscle has been deprived of oxygen for so long that it can be permanently damaged, in some cases causing death. There are treatments available in hospital that can prevent heart attacks and save lives, so if you have chest pain or symptoms of chest pain that last for more than 20 minutes, you should call an ambulance and be taken to hospital as soon as possible. Am I likely to have coronary artery disease? There are several risk factors that are proven to be associated with this disease. Even if you don’t have any of the following, it could still happen to you. You are more likely to have coronary artery disease if you have any of the following: Are or have been a smoker Diabetes High blood pressure (hypertension) High cholesterol A family history of coronary artery disease Are older (your risk increases as you get older) Treatment consists of medications to protect the heart and its blood vessels. These include Aspirin which makes the blood less sticky and prone to clots, medication to lower your cholesterol (even if it isn’t very high this is still helpful), medication to make your heart beat more slowly and to open the blood vessels. You will be given a Glyceryl Trinitrate (GTN) spray to carry with you with instructions of what to do if you have angina. You will be given advice on dietary changes that can protect the heart as well as stop smoking programmes. If you have had a heart attack you will be offered cardiac rehabilitation classes with a Specialist Cardiac Rehabilitation Nurse. Depending on test results, you may be offered procedures to either percutaneously (through the skin) or surgically correct the narrowed coronary arteries.
Patient information: This refers to narrowing of the arteries that supply blood to the heart muscle. The heart, like all other organs in the body, needs a constant supply of oxygen and energy. Narrowed arteries are unable to keep up with the demand needed to supply the heart muscle with blood and oxygen. A coronary artery narrowing (stenosis) or obstruction can cause damage to the heart muscle. The most common symptom of this problem is chest pain or tightness that occurs when you exert yourself (angina). Typical angina chest pain is a heavy sensation in your chest associated with shortness of breath. The pain sometimes radiates to your arms and can make you feel nauseated, breathless, dizzy or sweaty. Not everybody experiences the same sensation and any one of those symptoms can represent angina. If your GP thinks you may have angina, they will refer you for an assessment to plan treatment. Heart Attack (Myocardial Infarction) If an attack of chest pain lasts for more than 20 minutes, then you may be having a heart attack. This is when a piece of the heart muscle has been deprived of oxygen for so long that it can be permanently damaged, in some cases causing death. There are treatments available in hospital that can prevent heart attacks and save lives, so if you have chest pain or symptoms of chest pain that last for more than 20 minutes, you should call an ambulance and be taken to hospital as soon as possible. Am I likely to have coronary artery disease? There are several risk factors that are proven to be associated with this disease. Even if you don’t have any of the following, it could still happen to you. You are more likely to have coronary artery disease if you have any of the following: Are or have been a smoker Diabetes High blood pressure (hypertension) High cholesterol A family history of coronary artery disease Are older (your risk increases as you get older) Treatment consists of medications to protect the heart and its blood vessels. These include Aspirin which makes the blood less sticky and prone to clots, medication to lower your cholesterol (even if it isn’t very high this is still helpful), medication to make your heart beat more slowly and to open the blood vessels. You will be given a Glyceryl Trinitrate (GTN) spray to carry with you with instructions of what to do if you have angina. You will be given advice on dietary changes that can protect the heart as well as stop smoking programmes. If you have had a heart attack you will be offered cardiac rehabilitation classes with a Specialist Cardiac Rehabilitation Nurse. Depending on test results, you may be offered procedures to either percutaneously (through the skin) or surgically correct the narrowed coronary arteries.
The most common symptom of this problem is chest pain or tightness that occurs when you exert yourself (angina). Typical angina chest pain is a heavy sensation in your chest associated with shortness of breath. The pain sometimes radiates to your arms and can make you feel nauseated, breathless, dizzy or sweaty. Not everybody experiences the same sensation and any one of those symptoms can represent angina. If your GP thinks you may have angina, they will refer you for an assessment to plan treatment.
Am I likely to have coronary artery disease?
- Are or have been a smoker
- Diabetes
- High blood pressure (hypertension)
- High cholesterol
- A family history of coronary artery disease
- Are older (your risk increases as you get older)
Patient information: Heart failure refers to the heart failing to pump efficiently. There are many diseases that cause this including coronary artery disease, high blood pressure, viral infections, alcohol, and diseases affecting the valves of the heart. When the heart is inefficient a number of symptoms occur depending on the cause and severity of the condition. The main symptoms are tiredness, breathlessness on exertion or lying flat, and ankle swelling. Doctors often refer to oedema, which means fluid retention, usually in your feet or lungs, as a result of the heart not pumping efficiently. Tests looking for possible causes of heart failure include: Chest X-ray Blood tests to rule out iron overload (haemochromatosis) Electrocardiogram (ECG) Echocardiogram (Cardiac ultrasound or Echo) Coronary Angiogram Treatment You are likely to have several medications over time; these include medication to control the amount of fluid that builds up (diuretics), medication to protect your heart and slow it down as well as to thin your blood. You will be given advice about restricting the amount of sodium (salt) you take, as this can contribute to fluid retention and worsening symptoms. You can also be involved in cardiac rehabilitation programmes run by the cardiac nurses. You will be given reading material to learn more about your disease.
Patient information: Heart failure refers to the heart failing to pump efficiently. There are many diseases that cause this including coronary artery disease, high blood pressure, viral infections, alcohol, and diseases affecting the valves of the heart. When the heart is inefficient a number of symptoms occur depending on the cause and severity of the condition. The main symptoms are tiredness, breathlessness on exertion or lying flat, and ankle swelling. Doctors often refer to oedema, which means fluid retention, usually in your feet or lungs, as a result of the heart not pumping efficiently. Tests looking for possible causes of heart failure include: Chest X-ray Blood tests to rule out iron overload (haemochromatosis) Electrocardiogram (ECG) Echocardiogram (Cardiac ultrasound or Echo) Coronary Angiogram Treatment You are likely to have several medications over time; these include medication to control the amount of fluid that builds up (diuretics), medication to protect your heart and slow it down as well as to thin your blood. You will be given advice about restricting the amount of sodium (salt) you take, as this can contribute to fluid retention and worsening symptoms. You can also be involved in cardiac rehabilitation programmes run by the cardiac nurses. You will be given reading material to learn more about your disease.
Patient information:
Heart failure refers to the heart failing to pump efficiently.
There are many diseases that cause this including coronary artery disease, high blood pressure, viral infections, alcohol, and diseases affecting the valves of the heart. When the heart is inefficient a number of symptoms occur depending on the cause and severity of the condition. The main symptoms are tiredness, breathlessness on exertion or lying flat, and ankle swelling. Doctors often refer to oedema, which means fluid retention, usually in your feet or lungs, as a result of the heart not pumping efficiently.
Tests looking for possible causes of heart failure include:
- Chest X-ray
- Blood tests to rule out iron overload (haemochromatosis)
- Electrocardiogram (ECG)
- Echocardiogram (Cardiac ultrasound or Echo)
- Coronary Angiogram
Treatment
You are likely to have several medications over time; these include medication to control the amount of fluid that builds up (diuretics), medication to protect your heart and slow it down as well as to thin your blood. You will be given advice about restricting the amount of sodium (salt) you take, as this can contribute to fluid retention and worsening symptoms. You can also be involved in cardiac rehabilitation programmes run by the cardiac nurses. You will be given reading material to learn more about your disease.
Patient information: With any patient or doctor concern about the possibility of inflammatory myocarditis or pericarditis related to COVID-19 vaccination or any other cause, we can undertake an urgent cardiac ultrasound (Echocardiogram).
Patient information: With any patient or doctor concern about the possibility of inflammatory myocarditis or pericarditis related to COVID-19 vaccination or any other cause, we can undertake an urgent cardiac ultrasound (Echocardiogram).
Patient information:
With any patient or doctor concern about the possibility of inflammatory myocarditis or pericarditis related to COVID-19 vaccination or any other cause, we can undertake an urgent cardiac ultrasound (Echocardiogram).
Patient information: The four chambers of your heart receive and send blood to the lungs and body. Disorders affecting valves can either cause stenosis (a narrowing) or regurgitation (leakage after the valve has closed). Depending on what valve is involved, and how severe the damage is, it may result in symptoms of heart failure (see above), as it makes the heart pump inefficiently. Suspicion of a heart valve problem is usually picked up by your doctor when they listen to your heart and hear a heart murmur. A murmur is heard with the stethoscope and is related to turbulence of blood flow that occurs through a narrowed or leaky valve. Not all heart murmurs mean serious problems but are best investigated further. The chest x-ray, echocardiogram and ECG are the main tests to diagnose what valve is involved, the severity of the valve lesion and the effect on the heart. Treatment depends on the type and severity of the valve lesion. You may simply be monitored over years to see if anything changes. Some conditions require medication to thin the blood or treat any complicating heart problems. You may be referred to a heart surgeon for consideration of a valve replacement, repair or dilatation of a narrowed valve.
Patient information: The four chambers of your heart receive and send blood to the lungs and body. Disorders affecting valves can either cause stenosis (a narrowing) or regurgitation (leakage after the valve has closed). Depending on what valve is involved, and how severe the damage is, it may result in symptoms of heart failure (see above), as it makes the heart pump inefficiently. Suspicion of a heart valve problem is usually picked up by your doctor when they listen to your heart and hear a heart murmur. A murmur is heard with the stethoscope and is related to turbulence of blood flow that occurs through a narrowed or leaky valve. Not all heart murmurs mean serious problems but are best investigated further. The chest x-ray, echocardiogram and ECG are the main tests to diagnose what valve is involved, the severity of the valve lesion and the effect on the heart. Treatment depends on the type and severity of the valve lesion. You may simply be monitored over years to see if anything changes. Some conditions require medication to thin the blood or treat any complicating heart problems. You may be referred to a heart surgeon for consideration of a valve replacement, repair or dilatation of a narrowed valve.
Patient information:
The four chambers of your heart receive and send blood to the lungs and body.
Disorders affecting valves can either cause stenosis (a narrowing) or regurgitation (leakage after the valve has closed). Depending on what valve is involved, and how severe the damage is, it may result in symptoms of heart failure (see above), as it makes the heart pump inefficiently.
Suspicion of a heart valve problem is usually picked up by your doctor when they listen to your heart and hear a heart murmur. A murmur is heard with the stethoscope and is related to turbulence of blood flow that occurs through a narrowed or leaky valve. Not all heart murmurs mean serious problems but are best investigated further.
The chest x-ray, echocardiogram and ECG are the main tests to diagnose what valve is involved, the severity of the valve lesion and the effect on the heart.
Patient information: Your heart rate is controlled by an electrical system within the heart muscle. This system drives your heart to go faster when you exert yourself, and slower when you rest. A number of conditions can affect the heart rate or rhythm. Heart rate simply refers to how fast your heart is beating. Heart rhythm refers to the electrical source that is driving the heart rate, and whether or not it is regular or irregular. As some types of arrhythmias can cause you to faint without warning, your doctor may restrict your driving until the condition is controlled. Some common terms • Sinus rhythm is the normal rhythm • Dysrhythmia means abnormal rhythm • Fibrillation means irregular rhythm or quivering of one part of the heart • Bradycardia means slow heart rate (less than 60/minute) • Tachycardia means fast heart rate (more than 100/minute) • Paroxysmal means the arrhythmia is present only intermittently Tachycardia The most common form of this is atrial fibrillation. This is where your heart rhythm is irregular and often too fast. Symptoms include fatigue, palpitations (where you are aware of your heart racing or pounding), dizziness and breathlessness. Other tachycardias include supraventricular tachycardia (SVT) or ventricular tachycardia (VT). These have similar symptoms as atrial fibrillation but can also cause you to lose consciousness (blackout). Bradycardia A common form of this is related to electrical heart block. This occurs because messages from the electrical generator of the heart don't get through efficiently to the rest of the heart and hence it beats very slowly or can pause. Symptoms of the heart going too slowly include feeling tired, breathless or blacking out. Treatment Most treatments for tachycardias consist of medication to prevent the abnormal rhythm or make it slower, if and when it occurs. Atrial fibrillation can increase your risk of stroke, so blood-thinning medication is often used as well. If you have bradycardia you may be referred to an Auckland cardiologist for a permanent pacemaker. This is a small operation where a battery powered device is placed under the skin with wires that lead to your heart and provide it with electrical stimulation to prevent the heart from beating too slowly. You can't feel it doing this, but you will be aware of a small flat lump under your skin just below your collar bone.
Patient information: Your heart rate is controlled by an electrical system within the heart muscle. This system drives your heart to go faster when you exert yourself, and slower when you rest. A number of conditions can affect the heart rate or rhythm. Heart rate simply refers to how fast your heart is beating. Heart rhythm refers to the electrical source that is driving the heart rate, and whether or not it is regular or irregular. As some types of arrhythmias can cause you to faint without warning, your doctor may restrict your driving until the condition is controlled. Some common terms • Sinus rhythm is the normal rhythm • Dysrhythmia means abnormal rhythm • Fibrillation means irregular rhythm or quivering of one part of the heart • Bradycardia means slow heart rate (less than 60/minute) • Tachycardia means fast heart rate (more than 100/minute) • Paroxysmal means the arrhythmia is present only intermittently Tachycardia The most common form of this is atrial fibrillation. This is where your heart rhythm is irregular and often too fast. Symptoms include fatigue, palpitations (where you are aware of your heart racing or pounding), dizziness and breathlessness. Other tachycardias include supraventricular tachycardia (SVT) or ventricular tachycardia (VT). These have similar symptoms as atrial fibrillation but can also cause you to lose consciousness (blackout). Bradycardia A common form of this is related to electrical heart block. This occurs because messages from the electrical generator of the heart don't get through efficiently to the rest of the heart and hence it beats very slowly or can pause. Symptoms of the heart going too slowly include feeling tired, breathless or blacking out. Treatment Most treatments for tachycardias consist of medication to prevent the abnormal rhythm or make it slower, if and when it occurs. Atrial fibrillation can increase your risk of stroke, so blood-thinning medication is often used as well. If you have bradycardia you may be referred to an Auckland cardiologist for a permanent pacemaker. This is a small operation where a battery powered device is placed under the skin with wires that lead to your heart and provide it with electrical stimulation to prevent the heart from beating too slowly. You can't feel it doing this, but you will be aware of a small flat lump under your skin just below your collar bone.
Patient information:
Your heart rate is controlled by an electrical system within the heart muscle. This system drives your heart to go faster when you exert yourself, and slower when you rest.
A number of conditions can affect the heart rate or rhythm. Heart rate simply refers to how fast your heart is beating. Heart rhythm refers to the electrical source that is driving the heart rate, and whether or not it is regular or irregular. As some types of arrhythmias can cause you to faint without warning, your doctor may restrict your driving until the condition is controlled.
Some common terms
• Sinus rhythm is the normal rhythm
• Dysrhythmia means abnormal rhythm
• Fibrillation means irregular rhythm or quivering of one part of the heart
• Bradycardia means slow heart rate (less than 60/minute)
• Tachycardia means fast heart rate (more than 100/minute)
• Paroxysmal means the arrhythmia is present only intermittently
Tachycardia
The most common form of this is atrial fibrillation. This is where your heart rhythm is irregular and often too fast. Symptoms include fatigue, palpitations (where you are aware of your heart racing or pounding), dizziness and breathlessness. Other tachycardias include supraventricular tachycardia (SVT) or ventricular tachycardia (VT). These have similar symptoms as atrial fibrillation but can also cause you to lose consciousness (blackout).
Bradycardia
A common form of this is related to electrical heart block. This occurs because messages from the electrical generator of the heart don't get through efficiently to the rest of the heart and hence it beats very slowly or can pause. Symptoms of the heart going too slowly include feeling tired, breathless or blacking out.
Treatment
Most treatments for tachycardias consist of medication to prevent the abnormal rhythm or make it slower, if and when it occurs. Atrial fibrillation can increase your risk of stroke, so blood-thinning medication is often used as well. If you have bradycardia you may be referred to an Auckland cardiologist for a permanent pacemaker. This is a small operation where a battery powered device is placed under the skin with wires that lead to your heart and provide it with electrical stimulation to prevent the heart from beating too slowly. You can't feel it doing this, but you will be aware of a small flat lump under your skin just below your collar bone.
Patient information: Poorly treated hypertension can damage the heart, kidneys and increase the risk of heart failure, heart attack, renal failure, stroke and circulation problems to the lower limbs. We can assess BP both at rest and with exercise. We have Ambulatory Blood Pressure Monitoring and Echocardiography to assess the presence or absence of left ventricular hypertrophy, systolic and diastolic function. White coat hypertension can be recognised. We can exclude secondary hypertension and assess the contributors to high blood pressure and help with the appropriate management of difficult to treat hypertension with a combination of lifestyle change, diet and medications.
Patient information: Poorly treated hypertension can damage the heart, kidneys and increase the risk of heart failure, heart attack, renal failure, stroke and circulation problems to the lower limbs. We can assess BP both at rest and with exercise. We have Ambulatory Blood Pressure Monitoring and Echocardiography to assess the presence or absence of left ventricular hypertrophy, systolic and diastolic function. White coat hypertension can be recognised. We can exclude secondary hypertension and assess the contributors to high blood pressure and help with the appropriate management of difficult to treat hypertension with a combination of lifestyle change, diet and medications.
Patient information:
Poorly treated hypertension can damage the heart, kidneys and increase the risk of heart failure, heart attack, renal failure, stroke and circulation problems to the lower limbs.
We can assess BP both at rest and with exercise. We have Ambulatory Blood Pressure Monitoring and Echocardiography to assess the presence or absence of left ventricular hypertrophy, systolic and diastolic function.
White coat hypertension can be recognised.
We can exclude secondary hypertension and assess the contributors to high blood pressure and help with the appropriate management of difficult to treat hypertension with a combination of lifestyle change, diet and medications.
Patient information: Symptoms of asthma include cough, wheezing, a tight chest and trouble breathing. Asthma occurs when the main breathing tubes of your lungs are over-sensitive and react to things that don’t affect other people. As a result of this they become swollen, spasm, narrow and plug with mucus. If your asthma is not getting better with standard treatment (preventer and reliever inhalers) or if you are having more asthma attacks than you or your doctor are comfortable with, you may be referred to a specialist. In most cases you’ll be asked to give a complete medical history and will also be examined by the doctor. Sometimes other conditions can appear like asthma or complicate asthma, so you may be asked to have some tests to help in the diagnosis. Tests looking for severity and complicating features of asthma include: chest x-ray, spirometry, detailed lung function and CT chest scan. Treatment This includes the avoidance and management of triggers, taking medicines as well as changing some lifestyle factors. A peak flow meter can be used to keep a watch on your asthma and help with plans to prevent attacks. Stopping smoking is very important as is learning to recognise and avoid any trigger that precipitates your asthma attack. Asthma is treated with inhaled medicines. There are two types: 1. a preventer medicine is taken every day. It soothes the irritated breathing tubes and prevents worsening of asthma, “asthma attacks”. 2. a reliever treats the asthma attacks. It relaxes the tightened muscles around the breathing tubes. The aim is to find the least treatment that keeps your asthma well controlled.
Patient information: Symptoms of asthma include cough, wheezing, a tight chest and trouble breathing. Asthma occurs when the main breathing tubes of your lungs are over-sensitive and react to things that don’t affect other people. As a result of this they become swollen, spasm, narrow and plug with mucus. If your asthma is not getting better with standard treatment (preventer and reliever inhalers) or if you are having more asthma attacks than you or your doctor are comfortable with, you may be referred to a specialist. In most cases you’ll be asked to give a complete medical history and will also be examined by the doctor. Sometimes other conditions can appear like asthma or complicate asthma, so you may be asked to have some tests to help in the diagnosis. Tests looking for severity and complicating features of asthma include: chest x-ray, spirometry, detailed lung function and CT chest scan. Treatment This includes the avoidance and management of triggers, taking medicines as well as changing some lifestyle factors. A peak flow meter can be used to keep a watch on your asthma and help with plans to prevent attacks. Stopping smoking is very important as is learning to recognise and avoid any trigger that precipitates your asthma attack. Asthma is treated with inhaled medicines. There are two types: 1. a preventer medicine is taken every day. It soothes the irritated breathing tubes and prevents worsening of asthma, “asthma attacks”. 2. a reliever treats the asthma attacks. It relaxes the tightened muscles around the breathing tubes. The aim is to find the least treatment that keeps your asthma well controlled.
Patient information:
Symptoms of asthma include cough, wheezing, a tight chest and trouble breathing.
Asthma occurs when the main breathing tubes of your lungs are over-sensitive and react to things that don’t affect other people. As a result of this they become swollen, spasm, narrow and plug with mucus.
If your asthma is not getting better with standard treatment (preventer and reliever inhalers) or if you are having more asthma attacks than you or your doctor are comfortable with, you may be referred to a specialist.
In most cases you’ll be asked to give a complete medical history and will also be examined by the doctor. Sometimes other conditions can appear like asthma or complicate asthma, so you may be asked to have some tests to help in the diagnosis.
Tests looking for severity and complicating features of asthma include: chest x-ray, spirometry, detailed lung function and CT chest scan.
Treatment
This includes the avoidance and management of triggers, taking medicines as well as changing some lifestyle factors.
A peak flow meter can be used to keep a watch on your asthma and help with plans to prevent attacks. Stopping smoking is very important as is learning to recognise and avoid any trigger that precipitates your asthma attack.
Asthma is treated with inhaled medicines. There are two types:
1. a preventer medicine is taken every day. It soothes the irritated breathing tubes and prevents worsening of asthma, “asthma attacks”.
2. a reliever treats the asthma attacks. It relaxes the tightened muscles around the breathing tubes.
The aim is to find the least treatment that keeps your asthma well controlled.
Patient information: In COPD, the major feature is a lack of full reversibility in airflow obstruction. Airways collapse, become blocked and lung tissue and air sacs become damaged. COPD includes conditions such as emphysema, chronic bronchitis and chronic asthma. COPD is a long term and sometimes fatal disease that can be managed and slowed down. Smoking is the main cause of emphysema and chronic bronchitis. The term COPD covers a wide range of severity, from mild to very severe. Breathlessness on exertion, cough and sputum are the main symptoms. Recurrent chest infections can occur, setting off severe attacks of breathlessness. Chronic bronchitis is an inflammation of the main breathing tubes (bronchi) in the lungs, which results in the ongoing production of excess mucous (phlegm). There is often an associated reduction in the amount of airflow out of the lungs. In the early stages of chronic bronchitis, a cough usually occurs in the morning. As the disease progresses, coughing persists throughout the day. There is often associated shortness of breath and an increased rate of chest infections. Emphysema is the gradual destruction of the air sacs (alveoli) in the lungs. The alveoli are unable to completely relax. As they become larger they are not as good at transporting oxygen to the blood. Emphysema cannot be cured, but can be managed through medication and lifestyle changes and occasionally with surgery. Investigations: You may have some of the following tests before or after your clinic appointment: chest x-ray, spirometry, lung function tests, CT chest scan. Dr Kennedy will decide if you need any of these tests, depending on your symptoms and examination findings. Treatment: There are ways to manage COPD. The first and most important is to stop smoking if this applies to you. There are exercises and dietary changes that can help maintain and improve fitness. Being close to your ideal weight is always an advantage. Doing as much exercise as the condition allows and having the right calorie intake are important. Being very underweight can be as bad as being very overweight. There are a variety of medications and devices to deliver them. Making sure that doses of inhaled medications actually get to the airways is crucial. Sometimes it takes time to identify the best medication and delivery system. If you have COPD it is a good idea to have the flu vaccination every year and a pneumonia vaccine every 5 years.
Patient information: In COPD, the major feature is a lack of full reversibility in airflow obstruction. Airways collapse, become blocked and lung tissue and air sacs become damaged. COPD includes conditions such as emphysema, chronic bronchitis and chronic asthma. COPD is a long term and sometimes fatal disease that can be managed and slowed down. Smoking is the main cause of emphysema and chronic bronchitis. The term COPD covers a wide range of severity, from mild to very severe. Breathlessness on exertion, cough and sputum are the main symptoms. Recurrent chest infections can occur, setting off severe attacks of breathlessness. Chronic bronchitis is an inflammation of the main breathing tubes (bronchi) in the lungs, which results in the ongoing production of excess mucous (phlegm). There is often an associated reduction in the amount of airflow out of the lungs. In the early stages of chronic bronchitis, a cough usually occurs in the morning. As the disease progresses, coughing persists throughout the day. There is often associated shortness of breath and an increased rate of chest infections. Emphysema is the gradual destruction of the air sacs (alveoli) in the lungs. The alveoli are unable to completely relax. As they become larger they are not as good at transporting oxygen to the blood. Emphysema cannot be cured, but can be managed through medication and lifestyle changes and occasionally with surgery. Investigations: You may have some of the following tests before or after your clinic appointment: chest x-ray, spirometry, lung function tests, CT chest scan. Dr Kennedy will decide if you need any of these tests, depending on your symptoms and examination findings. Treatment: There are ways to manage COPD. The first and most important is to stop smoking if this applies to you. There are exercises and dietary changes that can help maintain and improve fitness. Being close to your ideal weight is always an advantage. Doing as much exercise as the condition allows and having the right calorie intake are important. Being very underweight can be as bad as being very overweight. There are a variety of medications and devices to deliver them. Making sure that doses of inhaled medications actually get to the airways is crucial. Sometimes it takes time to identify the best medication and delivery system. If you have COPD it is a good idea to have the flu vaccination every year and a pneumonia vaccine every 5 years.
Patient information:
In COPD, the major feature is a lack of full reversibility in airflow obstruction. Airways collapse, become blocked and lung tissue and air sacs become damaged.
COPD includes conditions such as emphysema, chronic bronchitis and chronic asthma. COPD is a long term and sometimes fatal disease that can be managed and slowed down. Smoking is the main cause of emphysema and chronic bronchitis.
The term COPD covers a wide range of severity, from mild to very severe. Breathlessness on exertion, cough and sputum are the main symptoms. Recurrent chest infections can occur, setting off severe attacks of breathlessness.
Chronic bronchitis is an inflammation of the main breathing tubes (bronchi) in the lungs, which results in the ongoing production of excess mucous (phlegm). There is often an associated reduction in the amount of airflow out of the lungs. In the early stages of chronic bronchitis, a cough usually occurs in the morning. As the disease progresses, coughing persists throughout the day. There is often associated shortness of breath and an increased rate of chest infections.
Emphysema is the gradual destruction of the air sacs (alveoli) in the lungs. The alveoli are unable to completely relax. As they become larger they are not as good at transporting oxygen to the blood. Emphysema cannot be cured, but can be managed through medication and lifestyle changes and occasionally with surgery.
Investigations:
You may have some of the following tests before or after your clinic appointment: chest x-ray, spirometry, lung function tests, CT chest scan. Dr Kennedy will decide if you need any of these tests, depending on your symptoms and examination findings.
Treatment:
There are ways to manage COPD. The first and most important is to stop smoking if this applies to you. There are exercises and dietary changes that can help maintain and improve fitness. Being close to your ideal weight is always an advantage. Doing as much exercise as the condition allows and having the right calorie intake are important. Being very underweight can be as bad as being very overweight.
If you have COPD it is a good idea to have the flu vaccination every year and a pneumonia vaccine every 5 years.
Patient information: Peptic ulcers are sores or eroded areas that form in the lining of the upper digestive tract. They usually occur in the oesophagus (oesophageal ulcer), stomach (gastric ulcer) or in the duodenum (duodenal ulcer) which is the first part of the small intestine. People with peptic ulcers can have a wide variety of symptoms and signs. At times they can be completely symptom-free or, much less commonly, can develop potentially life-threatening complications such as bleeding. Signs and symptoms of ulcers include: pain / burning or discomfort (usually in the upper abdomen) bloating an early sense of fullness with eating lack of appetite nausea vomiting bleeding, which is made apparent by blood in the stool, either in noticeable or microscopic amounts (very brisk bleeding will result in melaena with black and tarry stools that smell bad). Smoking, alcohol, anti-inflammatory medication and aspirin increase the risk of developing ulcers. Psychological stress and dietary factors (once thought to be the cause of ulcers) do not appear to have a major role in their development. Helicobacter pylori, a bacteria that is frequently found in the stomach is a major cause of stomach ulcers. If this is found when you have a gastric or duodenal ulcer, you will be given a course of antibiotics. The diagnosis is made by the history, examination and sometimes blood tests. You may be asked to have a gastroscopy (see above) to clarify the diagnosis and aid with treatment. Treatment consists of medication to reduce the amount of acid in the stomach which aids in the healing of ulcers and avoidance of any factor that may have caused the ulcers in the first place.
Patient information: Peptic ulcers are sores or eroded areas that form in the lining of the upper digestive tract. They usually occur in the oesophagus (oesophageal ulcer), stomach (gastric ulcer) or in the duodenum (duodenal ulcer) which is the first part of the small intestine. People with peptic ulcers can have a wide variety of symptoms and signs. At times they can be completely symptom-free or, much less commonly, can develop potentially life-threatening complications such as bleeding. Signs and symptoms of ulcers include: pain / burning or discomfort (usually in the upper abdomen) bloating an early sense of fullness with eating lack of appetite nausea vomiting bleeding, which is made apparent by blood in the stool, either in noticeable or microscopic amounts (very brisk bleeding will result in melaena with black and tarry stools that smell bad). Smoking, alcohol, anti-inflammatory medication and aspirin increase the risk of developing ulcers. Psychological stress and dietary factors (once thought to be the cause of ulcers) do not appear to have a major role in their development. Helicobacter pylori, a bacteria that is frequently found in the stomach is a major cause of stomach ulcers. If this is found when you have a gastric or duodenal ulcer, you will be given a course of antibiotics. The diagnosis is made by the history, examination and sometimes blood tests. You may be asked to have a gastroscopy (see above) to clarify the diagnosis and aid with treatment. Treatment consists of medication to reduce the amount of acid in the stomach which aids in the healing of ulcers and avoidance of any factor that may have caused the ulcers in the first place.
- pain / burning or discomfort (usually in the upper abdomen)
- bloating
- an early sense of fullness with eating
- lack of appetite
- nausea
- vomiting
- bleeding, which is made apparent by blood in the stool, either in noticeable or microscopic amounts (very brisk bleeding will result in melaena with black and tarry stools that smell bad).
Patient information: Coeliac disease is quite a common condition caused by gluten allergy. It affects up to 1 in 80 of the population. It is important to ensure the diagnosis before needing to commit to lifelong exclusion of gluten intake. The diagnosis is usually confirmed with blood tests and duodenal biopsies taken at gastroscopy. It is important that a gluten containing diet has been consumed, ideally four slices of bread a day for 8 weeks prior to the gastroscopy and duodenal biopsies. Coeliac disease can be associated with nutritional deficiencies (such as iron, folic acid and vitamin deficiencies) and a variety of unusual complications affecting the skin, joints and various other parts of the body. There is an increased risk of type I diabetes mellitus, thyroid disease and some cancers in those with untreated coeliac disease. After Specialist Dietitian advice, and contact with the New Zealand Coeliac Society, coeliac disease is usually well controlled with gluten exclusion from the diet. The risk of associated complications is reduced with the exclusion of gluten. A follow-up gastroscopy and repeat blood tests are often performed some time after commencing gluten exclusion, to ensure that an improvement is seen in the histological appearances. In the first instance, a further dietary review is arranged if the appearances are unsatisfactory.
Patient information: Coeliac disease is quite a common condition caused by gluten allergy. It affects up to 1 in 80 of the population. It is important to ensure the diagnosis before needing to commit to lifelong exclusion of gluten intake. The diagnosis is usually confirmed with blood tests and duodenal biopsies taken at gastroscopy. It is important that a gluten containing diet has been consumed, ideally four slices of bread a day for 8 weeks prior to the gastroscopy and duodenal biopsies. Coeliac disease can be associated with nutritional deficiencies (such as iron, folic acid and vitamin deficiencies) and a variety of unusual complications affecting the skin, joints and various other parts of the body. There is an increased risk of type I diabetes mellitus, thyroid disease and some cancers in those with untreated coeliac disease. After Specialist Dietitian advice, and contact with the New Zealand Coeliac Society, coeliac disease is usually well controlled with gluten exclusion from the diet. The risk of associated complications is reduced with the exclusion of gluten. A follow-up gastroscopy and repeat blood tests are often performed some time after commencing gluten exclusion, to ensure that an improvement is seen in the histological appearances. In the first instance, a further dietary review is arranged if the appearances are unsatisfactory.
Patient information:
Coeliac disease is quite a common condition caused by gluten allergy. It affects up to 1 in 80 of the population. It is important to ensure the diagnosis before needing to commit to lifelong exclusion of gluten intake. The diagnosis is usually confirmed with blood tests and duodenal biopsies taken at gastroscopy. It is important that a gluten containing diet has been consumed, ideally four slices of bread a day for 8 weeks prior to the gastroscopy and duodenal biopsies. Coeliac disease can be associated with nutritional deficiencies (such as iron, folic acid and vitamin deficiencies) and a variety of unusual complications affecting the skin, joints and various other parts of the body. There is an increased risk of type I diabetes mellitus, thyroid disease and some cancers in those with untreated coeliac disease.
After Specialist Dietitian advice, and contact with the New Zealand Coeliac Society, coeliac disease is usually well controlled with gluten exclusion from the diet. The risk of associated complications is reduced with the exclusion of gluten.
A follow-up gastroscopy and repeat blood tests are often performed some time after commencing gluten exclusion, to ensure that an improvement is seen in the histological appearances. In the first instance, a further dietary review is arranged if the appearances are unsatisfactory.
Patient information: This is inflammation of the liver, caused by a variety of different processes. Excess weight, cholesterol and diabetes can cause fatty liver which may in some cases cause hepatitis or inflammation in the liver. Autoimmune liver disease and iron overload can cause inflammation of the liver. Alcohol can affect the liver and cause inflammation which, in the long term, can damage the liver permanently. Hepatitis B and C are viruses that can cause chronic (long term) inflammation and damage to the liver. These viruses are passed from person to person through body fluids. For more information about Hepatitis B and C and their treatment see https://www.hepatitisfoundation.org.nz/ . Dr Kennedy does not offer a private service for viral liver disease.
Patient information: This is inflammation of the liver, caused by a variety of different processes. Excess weight, cholesterol and diabetes can cause fatty liver which may in some cases cause hepatitis or inflammation in the liver. Autoimmune liver disease and iron overload can cause inflammation of the liver. Alcohol can affect the liver and cause inflammation which, in the long term, can damage the liver permanently. Hepatitis B and C are viruses that can cause chronic (long term) inflammation and damage to the liver. These viruses are passed from person to person through body fluids. For more information about Hepatitis B and C and their treatment see https://www.hepatitisfoundation.org.nz/ . Dr Kennedy does not offer a private service for viral liver disease.
Patient information:
Excess weight, cholesterol and diabetes can cause fatty liver which may in some cases cause hepatitis or inflammation in the liver.
Autoimmune liver disease and iron overload can cause inflammation of the liver.
Alcohol can affect the liver and cause inflammation which, in the long term, can damage the liver permanently.
Hepatitis B and C are viruses that can cause chronic (long term) inflammation and damage to the liver. These viruses are passed from person to person through body fluids. For more information about Hepatitis B and C and their treatment see https://www.hepatitisfoundation.org.nz/ . Dr Kennedy does not offer a private service for viral liver disease.
Patient information: Haemochromatosis is an hereditary condition in which excess iron is absorbed from the intestinal tract. This iron accumulates in tissues throughout the body including the liver, pancreas, heart and joints and can lead to symptoms and signs including arthritis, skin pigmentation, liver damage, heart failure, diabetes and sexual dysfunction. It is important to diagnose this condition as early treatment can help prevent complications. Tests include blood tests for increased iron levels and genetic testing. Treatment consists of the removal of excessive iron from the body by repeated removal of a fixed amount of blood (therapeutic phlebotomy). This is very like repeated blood donations and is carried out at the blood donor centre.
Patient information: Haemochromatosis is an hereditary condition in which excess iron is absorbed from the intestinal tract. This iron accumulates in tissues throughout the body including the liver, pancreas, heart and joints and can lead to symptoms and signs including arthritis, skin pigmentation, liver damage, heart failure, diabetes and sexual dysfunction. It is important to diagnose this condition as early treatment can help prevent complications. Tests include blood tests for increased iron levels and genetic testing. Treatment consists of the removal of excessive iron from the body by repeated removal of a fixed amount of blood (therapeutic phlebotomy). This is very like repeated blood donations and is carried out at the blood donor centre.
Patient information:
Haemochromatosis is an hereditary condition in which excess iron is absorbed from the intestinal tract. This iron accumulates in tissues throughout the body including the liver, pancreas, heart and joints and can lead to symptoms and signs including arthritis, skin pigmentation, liver damage, heart failure, diabetes and sexual dysfunction. It is important to diagnose this condition as early treatment can help prevent complications. Tests include blood tests for increased iron levels and genetic testing. Treatment consists of the removal of excessive iron from the body by repeated removal of a fixed amount of blood (therapeutic phlebotomy). This is very like repeated blood donations and is carried out at the blood donor centre.
Patient information: In most cases, headaches are not due to significant underlying problems. However, you may be referred to a specialist if your GP is worried about the nature of your headaches or you are having difficulty controlling them with standard treatment. Migraine headaches are repeated or recurrent headaches, often accompanied by other symptoms. They can be triggered by certain factors/events/foods. In some people, a visual disturbance called an aura happens before the headache starts. Other symptoms that may precede or accompany the headache include loss of appetite, nausea, vomiting, increased sweating, irritability, fatigue and intolerance of light or noise. The headache may last several hours to days. Prior to coming to clinic for review of headaches it is useful to keep a diary. Write down: when your headaches occurred, how severe they were, additional symptoms, what you've eaten, sleep patterns, menstrual cycles, any other possible factors. There is no cure for migraine headaches but treatment is aimed at: preventing migraines from occurring, stopping the migraine once early symptoms develop, and treating the symptoms of migraine (e.g. pain, nausea). On occasions a CT head or MRI scan is necessary for difficult headache.
Patient information: In most cases, headaches are not due to significant underlying problems. However, you may be referred to a specialist if your GP is worried about the nature of your headaches or you are having difficulty controlling them with standard treatment. Migraine headaches are repeated or recurrent headaches, often accompanied by other symptoms. They can be triggered by certain factors/events/foods. In some people, a visual disturbance called an aura happens before the headache starts. Other symptoms that may precede or accompany the headache include loss of appetite, nausea, vomiting, increased sweating, irritability, fatigue and intolerance of light or noise. The headache may last several hours to days. Prior to coming to clinic for review of headaches it is useful to keep a diary. Write down: when your headaches occurred, how severe they were, additional symptoms, what you've eaten, sleep patterns, menstrual cycles, any other possible factors. There is no cure for migraine headaches but treatment is aimed at: preventing migraines from occurring, stopping the migraine once early symptoms develop, and treating the symptoms of migraine (e.g. pain, nausea). On occasions a CT head or MRI scan is necessary for difficult headache.
Patient information:
In most cases, headaches are not due to significant underlying problems. However, you may be referred to a specialist if your GP is worried about the nature of your headaches or you are having difficulty controlling them with standard treatment. Migraine headaches are repeated or recurrent headaches, often accompanied by other symptoms. They can be triggered by certain factors/events/foods. In some people, a visual disturbance called an aura happens before the headache starts.
Other symptoms that may precede or accompany the headache include loss of appetite, nausea, vomiting, increased sweating, irritability, fatigue and intolerance of light or noise. The headache may last several hours to days.
Prior to coming to clinic for review of headaches it is useful to keep a diary. Write down: when your headaches occurred, how severe they were, additional symptoms, what you've eaten, sleep patterns, menstrual cycles, any other possible factors.
There is no cure for migraine headaches but treatment is aimed at: preventing migraines from occurring, stopping the migraine once early symptoms develop, and treating the symptoms of migraine (e.g. pain, nausea).
On occasions a CT head or MRI scan is necessary for difficult headache.
Patient information: The thyroid is a gland that sits in the front, and towards the bottom, of your neck. It is responsible for producing a hormone called thyroxine.Thyroxine has an important role in the body as it affects many organs including the heart, muscles and bones. Diseases that affect the thyroid can make it either overactive (producing too much thyroxine), underactive (not producing enough thyroxine) or enlarged (goitre). Tests Thyroid problems are usually picked up with a blood test but there are other tests you may have to work out why the problem has occurred. These include: an ultrasound scan. This is where a hand-held scanner head is passed over your thyroid gland and pictures are taken a nuclear medicine scan. This is where you are given something to drink that contains a substance that only goes to the thyroid gland. Although it is radioactive it does not damage you or anyone else. Pictures are then taken of the thyroid gland that give the doctor information about what might be causing the problem fine needle aspirate (FNA). This is where a surgeon puts a very fine needle (smaller than for a blood test) into the thyroid gland to take some cells to look at under the microscope.
Patient information: The thyroid is a gland that sits in the front, and towards the bottom, of your neck. It is responsible for producing a hormone called thyroxine.Thyroxine has an important role in the body as it affects many organs including the heart, muscles and bones. Diseases that affect the thyroid can make it either overactive (producing too much thyroxine), underactive (not producing enough thyroxine) or enlarged (goitre). Tests Thyroid problems are usually picked up with a blood test but there are other tests you may have to work out why the problem has occurred. These include: an ultrasound scan. This is where a hand-held scanner head is passed over your thyroid gland and pictures are taken a nuclear medicine scan. This is where you are given something to drink that contains a substance that only goes to the thyroid gland. Although it is radioactive it does not damage you or anyone else. Pictures are then taken of the thyroid gland that give the doctor information about what might be causing the problem fine needle aspirate (FNA). This is where a surgeon puts a very fine needle (smaller than for a blood test) into the thyroid gland to take some cells to look at under the microscope.
Patient information:
The thyroid is a gland that sits in the front, and towards the bottom, of your neck.
It is responsible for producing a hormone called thyroxine.Thyroxine has an important role in the body as it affects many organs including the heart, muscles and bones.
Diseases that affect the thyroid can make it either overactive (producing too much thyroxine), underactive (not producing enough thyroxine) or enlarged (goitre).
Tests
Thyroid problems are usually picked up with a blood test but there are other tests you may have to work out why the problem has occurred. These include:
- an ultrasound scan. This is where a hand-held scanner head is passed over your thyroid gland and pictures are taken
- a nuclear medicine scan. This is where you are given something to drink that contains a substance that only goes to the thyroid gland. Although it is radioactive it does not damage you or anyone else. Pictures are then taken of the thyroid gland that give the doctor information about what might be causing the problem
- fine needle aspirate (FNA). This is where a surgeon puts a very fine needle (smaller than for a blood test) into the thyroid gland to take some cells to look at under the microscope.
Patient information: Osteoporosis weakens and makes your bones more prone to breaking (fracture). Women are more likely than men to suffer from osteoporosis and as you get older you are more likely to develop osteoporosis. Tests: Osteoporosis can be diagnosed by measuring bone mineral density (BMD). This test involves taking x-rays (DEXA scan) of the bones in your spine, and femur. You will also be asked to have a blood test to look for reasons why you might have osteoporosis. Treatment: There is no cure for osteoporosis, but there are treatments that can improve bone strength and reduce your chances of you breaking a bone. If you are diagnosed with osteoporosis you may be prescribed several medications to improve your bone strength to reduce your risk of fracture. You will have follow-up either with your GP or specialist to make sure that the medication suits you. You will be given some more detailed reading about things you can do to help manage your osteoporosis and about the type of medication you are on.
Patient information: Osteoporosis weakens and makes your bones more prone to breaking (fracture). Women are more likely than men to suffer from osteoporosis and as you get older you are more likely to develop osteoporosis. Tests: Osteoporosis can be diagnosed by measuring bone mineral density (BMD). This test involves taking x-rays (DEXA scan) of the bones in your spine, and femur. You will also be asked to have a blood test to look for reasons why you might have osteoporosis. Treatment: There is no cure for osteoporosis, but there are treatments that can improve bone strength and reduce your chances of you breaking a bone. If you are diagnosed with osteoporosis you may be prescribed several medications to improve your bone strength to reduce your risk of fracture. You will have follow-up either with your GP or specialist to make sure that the medication suits you. You will be given some more detailed reading about things you can do to help manage your osteoporosis and about the type of medication you are on.
Patient information:
Osteoporosis weakens and makes your bones more prone to breaking (fracture).
Women are more likely than men to suffer from osteoporosis and as you get older you are more likely to develop osteoporosis.
Tests:
Osteoporosis can be diagnosed by measuring bone mineral density (BMD). This test involves taking x-rays (DEXA scan) of the bones in your spine, and femur. You will also be asked to have a blood test to look for reasons why you might have osteoporosis.
Treatment:
There is no cure for osteoporosis, but there are treatments that can improve bone strength and reduce your chances of you breaking a bone.
If you are diagnosed with osteoporosis you may be prescribed several medications to improve your bone strength to reduce your risk of fracture. You will have follow-up either with your GP or specialist to make sure that the medication suits you. You will be given some more detailed reading about things you can do to help manage your osteoporosis and about the type of medication you are on.
Patient information: These are systemic conditions of unknown cause that cause significant disability. Giant cell arteritis is a serious inflammation that involves medium and large sized arteries. There is an associated risk of sudden blindness, stroke and other artery and cardiac problems. Giant cell arteritis requires an urgent diagnosis with temporal artery biopsy. Polymyalgia rheumatica is a less worrying condition, though untreated can cause significant disability. Some patients have both giant cell arteritis and polymyalgia together. Both giant cell arteritis and polymyalgia rheumatica are typically managed with corticosteroid tablets over months or short years. Regular blood tests are required for monitoring. On occasions more powerful treatment with methotrexate is required.
Patient information: These are systemic conditions of unknown cause that cause significant disability. Giant cell arteritis is a serious inflammation that involves medium and large sized arteries. There is an associated risk of sudden blindness, stroke and other artery and cardiac problems. Giant cell arteritis requires an urgent diagnosis with temporal artery biopsy. Polymyalgia rheumatica is a less worrying condition, though untreated can cause significant disability. Some patients have both giant cell arteritis and polymyalgia together. Both giant cell arteritis and polymyalgia rheumatica are typically managed with corticosteroid tablets over months or short years. Regular blood tests are required for monitoring. On occasions more powerful treatment with methotrexate is required.
Patient information:
These are systemic conditions of unknown cause that cause significant disability. Giant cell arteritis is a serious inflammation that involves medium and large sized arteries. There is an associated risk of sudden blindness, stroke and other artery and cardiac problems. Giant cell arteritis requires an urgent diagnosis with temporal artery biopsy.
Polymyalgia rheumatica is a less worrying condition, though untreated can cause significant disability. Some patients have both giant cell arteritis and polymyalgia together. Both giant cell arteritis and polymyalgia rheumatica are typically managed with corticosteroid tablets over months or short years. Regular blood tests are required for monitoring. On occasions more powerful treatment with methotrexate is required.
Patient information: Gout is an acutely painful, disabling form of arthritis associated with the accumulation of monosodium urate crystals in the joints and soft tissues. With good treatment, acute episodes of gout can be controlled. Medications that exacerbate gout should be avoided to reduce the likelihood of further episodes of gout. Other exacerbants can be recognised and their intake minimised. More importantly, regular prophylactic treatment with carefully administered allopurinol can gradually be introduced to prevent destruction of the joints and the accumulation of urate in the tissues (tophi). Tophi can regress with treatment. Uric acid kidney stones can also be prevented in many cases.
Patient information: Gout is an acutely painful, disabling form of arthritis associated with the accumulation of monosodium urate crystals in the joints and soft tissues. With good treatment, acute episodes of gout can be controlled. Medications that exacerbate gout should be avoided to reduce the likelihood of further episodes of gout. Other exacerbants can be recognised and their intake minimised. More importantly, regular prophylactic treatment with carefully administered allopurinol can gradually be introduced to prevent destruction of the joints and the accumulation of urate in the tissues (tophi). Tophi can regress with treatment. Uric acid kidney stones can also be prevented in many cases.
Patient information:
Gout is an acutely painful, disabling form of arthritis associated with the accumulation of monosodium urate crystals in the joints and soft tissues.
With good treatment, acute episodes of gout can be controlled. Medications that exacerbate gout should be avoided to reduce the likelihood of further episodes of gout. Other exacerbants can be recognised and their intake minimised.
More importantly, regular prophylactic treatment with carefully administered allopurinol can gradually be introduced to prevent destruction of the joints and the accumulation of urate in the tissues (tophi). Tophi can regress with treatment.
Uric acid kidney stones can also be prevented in many cases.
Patient information: In RA the body’s immune system attacks the lining of the joints. This results in inflamed (red, hot, swollen), stiff and painful joints and eventually the destruction of the cartilage and bone of joints. RA can occur at any age. The cause is unknown. Symptoms do not only involve the joints but you may suffer from tiredness, low energy, fevers, poor appetite with weight loss and poor sleep. Diagnosis is made on the basis of your history and examination of your joints. X-rays may be normal in the early stages of the disease. MRI can be more sensitive at picking up early changes but can also be normal. Blood tests are done looking for an antibody that is present in about 75% of people with RA. This is called the rheumatoid factor. Unfortunately people who don’t have RA can have a positive rheumatoid factor test. Other blood tests can also help make the diagnosis. Treatment includes medications to relieve pain and inflammation. It also involves medication aiming at modifying the immune system to stop it from damaging the joints further. There are several medications in this group and your specialist will discuss side effects and benefits with you so you can work out which suit you best.
Patient information: In RA the body’s immune system attacks the lining of the joints. This results in inflamed (red, hot, swollen), stiff and painful joints and eventually the destruction of the cartilage and bone of joints. RA can occur at any age. The cause is unknown. Symptoms do not only involve the joints but you may suffer from tiredness, low energy, fevers, poor appetite with weight loss and poor sleep. Diagnosis is made on the basis of your history and examination of your joints. X-rays may be normal in the early stages of the disease. MRI can be more sensitive at picking up early changes but can also be normal. Blood tests are done looking for an antibody that is present in about 75% of people with RA. This is called the rheumatoid factor. Unfortunately people who don’t have RA can have a positive rheumatoid factor test. Other blood tests can also help make the diagnosis. Treatment includes medications to relieve pain and inflammation. It also involves medication aiming at modifying the immune system to stop it from damaging the joints further. There are several medications in this group and your specialist will discuss side effects and benefits with you so you can work out which suit you best.
Patient information: Symptoms include aches, pains, fatigue, morning stiffness and sleep problems. The diagnosis is made on the history of the pain and accompanying symptoms as well as the presence of tender (trigger) points at specific sites on the body. There are a number of different theories and reasons for this condition. There will often be blood tests and maybe x-rays to exclude other diagnoses. Treatment involves education, cognitive behavioural therapy, a graduated exercise programme, pain killers, rest and sometimes antidepressant medication.
Patient information: Symptoms include aches, pains, fatigue, morning stiffness and sleep problems. The diagnosis is made on the history of the pain and accompanying symptoms as well as the presence of tender (trigger) points at specific sites on the body. There are a number of different theories and reasons for this condition. There will often be blood tests and maybe x-rays to exclude other diagnoses. Treatment involves education, cognitive behavioural therapy, a graduated exercise programme, pain killers, rest and sometimes antidepressant medication.
Patient information:
Symptoms include aches, pains, fatigue, morning stiffness and sleep problems.
The diagnosis is made on the history of the pain and accompanying symptoms as well as the presence of tender (trigger) points at specific sites on the body. There are a number of different theories and reasons for this condition. There will often be blood tests and maybe x-rays to exclude other diagnoses. Treatment involves education, cognitive behavioural therapy, a graduated exercise programme, pain killers, rest and sometimes antidepressant medication.
Patient information: General Physicians specialise in the diagnosis of difficult conditions. Many of my referrals include patients with symptoms of weight loss, fatigue, headaches, breathing difficulties, generalised pain, etc. It is important to exclude serious disease with an appropriate history, examination and investigations. In many cases sinister pathology can be excluded, an explanation for symptoms can be found and reassurance provided.
Patient information: General Physicians specialise in the diagnosis of difficult conditions. Many of my referrals include patients with symptoms of weight loss, fatigue, headaches, breathing difficulties, generalised pain, etc. It is important to exclude serious disease with an appropriate history, examination and investigations. In many cases sinister pathology can be excluded, an explanation for symptoms can be found and reassurance provided.
Patient information:
General Physicians specialise in the diagnosis of difficult conditions. Many of my referrals include patients with symptoms of weight loss, fatigue, headaches, breathing difficulties, generalised pain, etc.
It is important to exclude serious disease with an appropriate history, examination and investigations.
In many cases sinister pathology can be excluded, an explanation for symptoms can be found and reassurance provided.
Disability Assistance
Wheelchair access
Document Downloads
- 24 or 48-Hour Cardiac Holter Monitoring (PDF, 106.6 KB)
- 24-Hour Blood Pressure Monitoring (ABPM) (PDF, 96.1 KB)
- Angina (PDF, 453.9 KB)
- Atrial Fibrillation (AF) (PDF, 3.7 MB)
- Coronary Angiography and Angioplasty (PCI) (PDF, 2.2 MB)
- Coronary Artery Bypass Graft Surgery (CABG) (PDF, 3 MB)
- Dobutamine Stress Echocardiogram (DSE) (PDF, 89.5 KB)
- Echocardiogram (TTE) (PDF, 110.1 KB)
- Electrocardiogram (ECG) (PDF, 129.2 KB)
- Event Monitoring (PDF, 95.7 KB)
- Exercise Tolerance Test (ETT) (PDF, 120.5 KB)
- Heart Failure (PDF, 5.3 MB)
- Heart Valve Disease (PDF, 1.1 MB)
- Hypertension (High Blood Pressure) (PDF, 895.2 KB)
- Implantable Cardioverter Defibrillator (ICD) (PDF, 1.8 MB)
- Pacemaker (PDF, 1.2 MB)
Visiting Hours
Clinics all day Tuesdays and Thursday mornings.
Travel Directions
Travelling from South
Travelling North on State Highway 1, at 74 Western Hills Drive, on left opposite St John Ambulance station.
Travelling from North
Travelling South on State Highway 1, at Western Hills Drive, on right, opposite St John Ambulance Station.
Public Transport
Parking
Off-street parking is available and there is ramp access for the disabled.
Accommodation
Pharmacy
The closest pharmacy (including after hours) is the Kensington Pharmacy at the Kensington Shopping Centre, only a couple of minutes drive from Western Hills Clinic. Other pharmacies close to the rooms on the way north are David's Pharmacy in Three Mile Bush Road and the Kamo Pharmacy in Kamo Road, both at the Kamo Shopping Centre.
Other
Arthritis New Zealand: arthritis.org.nz First Floor, 25 Rathbone St, Whangārei (09) 438 5037
Ascot Cardiology Auckland: 0800 4HEART 0800 443 278 ascotcardiologygroup.co.nz
Ascot Radiology Auckland :09 520 9550 www.ascotrad.co.nz ascotrad.co.nz
Asthma Foundation: asthmanz.co.nz
Coeliac Society New Zealand: coeliac.org.nz
EchoNorth: 56 Kamo Rd, Whangārei (09) 974 8844 echonorth.co.nz
GreenLane Imaging: 0800 CTSCAN 0800 287 226 ascotrad.co.nz
Multiple Sclerosis Society (Northland) Field Officer: 027 539 9883 (09) 438 3945 www.msnz.org.nz
National Heart Foundation: Level 1, 25 Rathbone Street, Whangārei (09) 459 6518 heartfoundation.org.nz
Northland Pathology Laboratory Collection Centres: norpath.co.nz
TRG: 11 Kensington Ave, Whangārei (09) 437 0540, Kerikeri (09) 407 6222 trgimaging.co.nz
Trinity MRI Auckland: trinitymri.co.nz
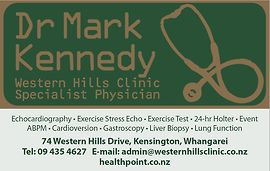
Contact Details
74 Western Hills Drive, Whangārei
Northland
8:00 AM to 4:30 PM.
-
Phone
(09) 435 4627 (Reception Tue - Fri)
-
Mobile
Emergency Phone (021) 702 395
Healthlink EDI
west74hc
Email
For any urgent Echocardiogram, Exercise Stress Echocardiogram or Exercise Tolerance Test, contact Clinic Nurse (Gemma) on (09) 435 4627 on Tuesday and Thursday. If she is unavailable, and it is URGENT, call Mark Kennedy on (021) 702 395. We can undertake Transthoracic Echocardiograms most weekdays.
Street Address
74 Western Hills Drive
Kensington
Whangārei
Northland 0112
Opposite St John Ambulance Station, SH 1.
Postal Address
Dr Mark Kennedy
Western Hills Clinic
74 Western Hills Drive
Kensington
Whangārei 0112
Was this page helpful?
This page was last updated at 12:10PM on December 9, 2024. This information is reviewed and edited by Dr Mark Kennedy - Private Internal Medicine Specialist.

