Northland > Private Hospitals & Specialists >
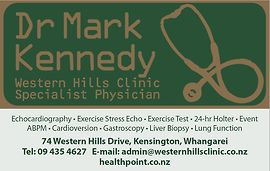
Dr Mark Kennedy - Private Internal Medicine Specialist
Private Service, Internal Medicine, Cardiology, Gastroenterology & Hepatology (Liver), Respiratory
Pleural Aspiration and Biopsy
Patient information:
Pleural aspiration and biopsy are most often undertaken to diagnose the cause for pleural fluid or pleural mass/thickening. These procedures are usually undertaken under local anaesthesia after ultrasound marking, or under CT guidance. Pleural aspiration and biopsy are performed to try and diagnose the cause of the problem such as inflammation, infection, tuberculosis or cancer.
Pleural aspiration and pleural biopsy:
These procedures can be done in different ways. A surgeon can perform them, usually thoracoscopically (i.e. 'key hole' surgery in which thin, rigid telescopes to which biopsy forceps or other instruments can be attached, are inserted through the chest wall). Thoracoscopy requires a general anaesthetic and one or more days in hospital.
Pleural aspiration and biopsy are usually undertaken under local anaesthetic and sedation, using a special needle which is much finer than the instruments a surgeon uses. Afterwards the patient has a chest X-ray and then returns home.
The best site for inserting the special needle is located beforehand by ultrasound (i.e. bouncing sound waves through the chest wall), confirming there is fluid at that site. Local anaesthetic is injected under the skin and then into the muscle at that site, before inserting the needle through which biopsies and fluid can be collected.
The procedure can take anything from 20 - 60 minutes, depending on how much fluid has to be removed. The aspiration and biopsy site are closed with a suture (i.e. a stitch) that needs to be removed about 5 days later by your GP.
Is pleural aspiration or pleural biopsy painful?
This depends to a large extent on the skill of the person doing the procedure. Performed by an expert, they should be pain-free or almost pain-free. If there is discomfort I will always do my best to minimise it.
Care is needed with very large pleural effusions (e.g. where there is more than 1.5 litres of fluid) or the effusion has been present for a long time. Rapid removal of fluid can cause pain or make breathing worse. In these situations it is sometimes better to insert a pleural tube/catheter and drain the fluid slowly over several hours, in hospital.
The doctor removing pleural fluid needs experience and patience.
Why is a pleural aspiration needed?
There are three main reasons:
- Firstly, to diagnose the cause of the pleural effusion.
- Secondly, to give relief from the breathlessness caused by a large pleural effusion.
- Lastly, to see whether, following the removal of most of the fluid, the lung has fully re-expanded and is sitting adjacent to the chest wall and the mediastinum (i.e. the tissues in the centre of the chest). This information is needed in the context of pleural effusion caused by a cancer. Sometimes recurrent pleural effusion caused by cancer can be eliminated by doing a 'pleurodesis'. This involves putting a chemical or talc into the pleural space (by a surgeon). However, this only works if the lung can fully re-expand against the chest wall. If the lung can re-expand, pleurodesis can be done.
After the procedure:
The results usually take a week or more to return. When the results are available, they are reviewed with you and management plan options are discussed in Dr Kennedy's rooms.